If you have any questions, you may call us at (314) 576-1400.
There are many young women today who are cancer survivors, but their remarkable cures have cost most of them their fertility. Bone marrow transplantations, modern radiation treatment, and aggressive chemotherapy permanently cures up to 90% of cancers in young women today, but their eggs and ovaries are either completely or partially destroyed by these treatments.
For many years (since 1994), scientists have been hoping that the ovaries of such patients could be removed and frozen before such cancer therapy destroys them, so that maybe in the future these cryopreserved ovaries could be transplanted back to the patients, and thus restore their fertility. Dr. Sherman Silber of St. Louis, Missouri [see video], demonstrates that this dream is now a robust reality.
Dr. Silber demonstrates this procedure for preserving fertility[see video] in a 31 year old woman who first saw him as a cancer patient at age 19. She was a 19 year old girl then about to undergo treatment for a severe case of Hodgkin’s’ lymphoma which her doctors told her would render her permanently sterile, and if she were cured of cancer, she would nonetheless become permanently menopausal, and never be able to have children. Dr. Silber warned her in 1997 that he could not predict at that time if it would indeed allow her to have children in the future, but it was her only chance, and at the young age of 19, she decided to take it, and it worked! Click here to hear Dr. Silber discuss this case on National Public Radio (NPR).
During the three years after her ovary was frozen by Dr. Silber, she wound up having several recurrences of her cancer, requiring two bone marrow transplants and many rounds of radiation and chemotherapy. But eventually she was cured and indeed, eleven years later she got married at age 31. Although she was prematurely menopausal, she still dreamed of having children of her own, which her cancer doctors had warned her, could never happen. Yet after she received a transplant of her ovarian tissue (which had been frozen 12 years earlier), she conceived a healthy child. Over 60 such young cancer patients have subsequently undergone freezing of eggs or ovarian tissue at the Infertility Center of St. Louis. Now it appears that their dreams will indeed come true.
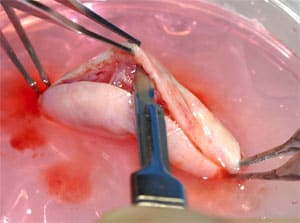
Meanwhile, Dr. Silber from 2003 until 2009 had performed a remarkable series of nine ovary transplants between very rare identical twin sisters who were discordant for premature ovarian failure (which means that one sister had gone into menopause early in life and the other identical twin sister was quite fertile). This unusual series of transplants produced 12 pregnancies in the eight otherwise sterile recipients who had Fallopian tubes, and eight healthy births (4 miscarriages). The technical innovations he had the opportunity to develop in such a series, clarified how the ovarian tissue needs to be frozen, thawed, and indeed transplanted, to get optimal results with cancer patients.
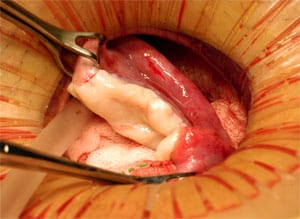
Next he performed transplantation of frozen ovarian tissue in patients who had been cured of their cancer, but had frozen their ovary tissue prior to their sterilizing cancer treatment,and achieved healthy pregnancies. Thus far all three frozen cases have been successful resulting in healthy babies. The technical video [see video] shows this entire technique, including patient interviews. It demonstrates that preserving fertility in cancer patients by freezing their ovarian tissue is now a reality.

The 31 year old cancer survivor told us, “You know, I feel so fortunate that I had cancer. My girlfriends in their 30’s are all worried about their biological clock, but I have a 19 year old ovary, and am, ironically even more fertile than they are.” Therefore this technique not only preserves the fertility of cancer patients, but also can protect non-cancer patients from the otherwise devastating effect of their biological clock.
By 2010, already 23 healthy babies have been born as a result of ovary tissue transplants, whether fresh or frozen. It is no longer therefore just an experimental procedure, but should be considered standard therapy to preserve fertility.
It is now officially recommended by the Cancer Society that all young men and women should be counseled on how to preserve their fertility before undergoing cancer treatment, as it is not necessary any longer for them to remain sterile as a result of their cancer therapy.
Yet there are still many sad stories we hear daily of young women who will never be able to have children because of backward views of their oncologist. Many otherwise well meaning oncologists do not want to bother with referring their patients for fertility preservation for fear it would delay their cancer treatment. But freezing a young woman’s ovarian tissue is a simple, minor procedure that will only delay treatment by 2 days, and will in no way hamper the cure of their cancer.
Just recently we consulted with the parents of a 17 year old girl with Hodgkin’s Disease who were thrilled to save their daughter’s fertility, but their oncologist actually talked them into not doing this and to only concentrate on her Hodgkin’s. She will consequently never have children. Contrast that girl’s sterile future to that of Amy and Melissa, who look forward in the future to having a family of their own.
Fertility Preservation with Ovary Transplantation
Several days ago, the first patient in the United States delivered a healthy baby from a transplanted ovary which had been frozen thirteen years ago, before she underwent otherwise sterilizing cancer treatment as a 19 year old girl. Dr. Silber’s paper published in Fertility and Sterility, provides otherwise rare information for guiding fertility preservation practices, and counseling patients about the likelihood of success of ovary transplantation. This is the largest series of ovarian transplants to date, with the largest number of pregnancies and live births, and the longest number of follow-up years to evaluate the efficacy of ovary transplantation, fresh or frozen, and the expected duration of function of the transplanted ovary.
After fresh or frozen ovary transplantation, these patients have essentially a completely normal pregnancy rate and delivery rate as would be expected in any normal group of women who had never had cancer or who had never required ovary transplantation to cure their premature menopause.
Ovarian tissue frozen to preserve fertility should be able to completely restore the fertility that the young woman would have had if she had never undergone otherwise sterilizing radiation and chemotherapy.
One in every 250 young women today are cancer survivors, but their cancer treatment usually has rendered them sterile. With the approach of ovarian tissue freezing and transplantation, their fertility can now be preserved, and rather inexpensively. Interestingly, most of these cancer survivors whose frozen ovarian tissue is stored with us, tell us that they felt “fortunate” that they were diagnosed with cancer. While this is an odd thing to say, they point out that their girlfriends in their 30’s are all worried about their biological clock, but these cancer survivors do not have to worry about that, because their frozen ovarian tissue is that of a teenager or woman in her 20’s, the time in their lives when their ovary tissue frozen.
One, therefore, has to consider whether this could be also be offered to young women who need to put off childbearing aspirations until they are in their late 30’s or 40’s, as so many women in our modern society must do. This presents an option for them to preserve their fertility, not against the consequences of cancer therapy, but against the slowly ticking away of their biological clocks.
Infertility is a huge and growing global epidemic, and the reason for this epidemic is the putting off of childbearing by so many modern women. In previous generations, the norm was to get married in our early 20’s and have all our children before age 30. At one time, you were considered to be really old at 65 if lucky enough to live that long. Now we all plan to be very healthy and active into our 80’s and, therefore, childbearing is put off until one’s late 30’s or early 40’s or even later. But a woman’s eggs still age and by the late 30’s, 50 percent of women are infertile. If ovary or egg freezing were offered to these women while they were still young, we could completely overcome this infertility epidemic.
During a campaign breakfast a few years ago, Dr. Silber had the wonderful opportunity to meet Hillary Clinton. In just a few minutes she found out about Dr. Silber’s work in infertility, running a large IVF program, and asked why there was so much more infertility nowadays. Dr. Silber explained about the biological clock and she asked what he was going to do to solve this problem. Dr. Silber told her about ovary and egg freezing at the Infertility Center of St. Louis, currently being used only for cancer patients, because of potential ethical questions about using this method “just” to prolong the fertility of women who do not have cancer. Her very direct and immediate answer to that was: “I THINK THIS IS A NO BRAINER. YOU SHOULD OFFER IT TO ANYONE, WITH OR WITHOUT CANCER.” So the ultimate implication of these findings is the availability to prolong the reproductive lifespan not only of cancer patients, but of any young woman who needs to postpone childbearing.
This method is about to be applied also to freezing ovarian tissue for younger pediatric-age patients who are pre-pubertal, which should work as well as for post-pubertal young women. The plan is to do the same with the testes of pre-pubertal boys who obviously cannot give us a sperm sample to freeze.



Egg or Embryo Freezing
Young women with cancer can also preserve their fertility by an IVF type procedure, retrieving individual eggs andfreezing the eggs (or fertilizing them, in the case of married women for example, and freezing the embryos). With this approach, the young woman with cancer can undergo hormonal stimulation for several weeks after day one of her next menstrual cycle, to mature 10 to 15 follicles and the doctors can retrieve eggs by ultrasound-guided needle aspiration, just like with IVF. If they have a permanent partner, the eggs can be fertilized and the resultant embryos (rather than just eggs) frozen. Some may prefer this approach to having ovarian tissue frozen.
The problem with this approach of egg or embryo freezing for cancer patients is that it could delay the cancer treatment by 4 to 8 weeks, or even longer, and the patient’s oncologist may not be willing to wait this long before initiating cancer treatment. Furthermore, like with any IVF procedure, the pregnancy rate per cycle is usually only 30% to 50%. So if she doesn’t get pregnant from these frozen eggs or embryos (derived from just this one retrieval cycle) then she has no further options because her ovaries have already been destroyed by the cancer treatment. With frozen ovary tissue, she will have hundreds of thousands of eggs frozen and many more years of opportunities for pregnancies and children. That is why for most cancer cases, it is preferable and easier on the patient to perform ovarian tissue freezing to preserve their fertility rather than simple egg freezing or IVF with embryo freezing.
The other problem with eggs or embryo freezing for many infertility centers is that the conventional freezing technologies which most IVF labs use are not reliable. With most of these conventional freezing technologies, the vast majority of eggs are damaged and as many as half the embryos are destroyed. To use this method of fertility preservation, it is absolutely critical for the IVF lab to be very experienced with “vitrification.”
Freezing Eggs or Embryos by the Vitrification Process

The classic problem with freezing eggs used to be that as one lowered the temperature below the freezing point, the egg’s genetic material would suffer damage due to ice crystals forming inside the cell. It was only possible to freeze embryos, in which the genetic material had already combined with that from the sperm, and stabilized. The classic freezing techniques (which have been known since 1983) were based on trying to extract water from the cell as the temperature drops, to minimize ice crystal damage. This has all changed now with the development of our new vitrification techniques. We no longer have to play a tenuous game of minimizing ice crystal formation — we can now entirely avoid it — so that there is no internal damage to the egg whatsoever.
This new technique of freezing called “vitrification” avoids the damage caused by ice forming inside the cell by not trying to pull every last molecule of water out, because it is impossible to do this 100%. In fact, 70% of the cell is water, and at best you can reduce that to 30%. So with the conventional controlled rate slow-freezing technique, there is always going to be some intra-cellular ice crystal formation, causing some damage to embryos, and severely damaging most eggs. Vitrification uses a super high concentration of antifreeze (DMSO and ethylene glycol), and drops the temperature so rapidly that the water inside the cell never becomes ice. It just instantaneously super-cools into a solid with no ice crystal formation at all.
We can now freeze and thaw, and even refreeze and rethaw, with impunity, using this new protocol from Dr. Masashige Kuwayama from the Kato Clinic in Tokyo. With conventional “slow freezing,” the temperature of the embryo goes down at precisely 0.3°C per minute. With vitrification (using four times the concentration of antifreeze, or cryoprotectant), the temperature is dropped at 23,000 degrees C° per minute, that is 70,000 times faster. At that speed of cooling, and at that concentration of antifreeze, ice crystals simply cannot form.
Of course, it is not quite as simple as it might sound. Such high concentrations of antifreeze, in a few minutes, could be toxic to cells. Therefore, the embryos (or eggs) must first be placed in lower concentrations of antifreeze (and sucrose to draw some water out), and then left in high concentrations only for less than a minute before instantaneous freezing. Then when the time comes to thaw the embryo, it must be instantaneously warmed, immediately taken out of the high concentration of antifreeze, and then placed into a solution with lower concentration, in order to avoid antifreeze toxicity. This requires more skill than conventional freezing, but it is faster, cheaper, and most importantly, avoids almost all freezing damage to either eggs or embryos. Such a reliable method of embryo freezing gives the IVF program much greater ability to safely preserve fertility.
Using this vitrification technique for freezing, we can reliably preserve eggs as well as embryos so that the pregnancy rate is no different than if the eggs or embryos had never been frozen. This allows us to preserve the fertility of young women for the future if they wish to delay childbearing, but not lose their fertility as they age. Without skill in vitrification, a clinic cannot give any assurance of the survival of any eggs or embryos they attempt to freeze to preserve the fertility of cancer patients.
See also:
- A Special Message From Dr. Silber About Your Biological Clock and Preserving Your Fertility
- News Coverage of a Whole Ovary Transplant
- Fertility expert Dr. Sherman Silber gives hope to infertile men and women
- Preserving Your Fertility
- Ovarian Tissue Freezing
- Egg, Embryo, and Sperm Freezing
- Freezing the Biological Clock
- Complex Surgery Involved In First Successful Whole Ovary Transplant [Article]
- Giving An Ovary To My Twin Was A ‘Magical’ Opportunity [Article]
Vitrification of Ovarian Tissue
Although conventional freezing of ovarian tissue has worked quite well since we began in 1996, it results in loss of half the eggs. Of course that still leaves 50,000 eggs that survive; so ovarian tissue freezing has been a robust technique for preserving fertility for well over a decade with many successful pregnancies. However, we can now use the vitrification technique of freezing also for ovarian tissue. This is truly a remarkable improvement for several reasons.
Firstly, with vitrification, we essentially LOSE NO EGGS. The frozen ovarian tissue with vitrification is no different from fresh tissue. This means that when the ovarian tissue is transplanted back (after the patient is cured of her cancer), it will have a completely normal lifetime of function. It should last twice as long as ovarian tissue that was cryopreserved with the conventional slow-freezing approach.
But there is a much more profound advantage to using the vitrification technique for freezing ovarian tissue for cancer patients. There are some cancers, like leukemia, that metastasize to all organs, including the ovary. So for leukemia patients (unlike Hodgkin’s and other solid tumors), the ovarian tissue cannot be transplanted back. For these patients the maturing follicles in the ovarian tissue can be cultured in vitro and successfully fertilized for IVF. With frozen tissue there will not just be a few eggs, but literally thousands of such eggs available for IVF.
The only problem is that conventional freezing of ovarian tissue destroys all of these maturing eggs and only spares the immature primordial follicles which cannot be cultured in vitro.
But vitrification of the ovarian tissue spares all of the follicles, even the maturing follicles, the ones which can be used for IVF. Thus with vitrification of ovarian tissue, even cancer patients with leukemia can have successful preservation of their fertility.
Ultimately, it is usually better to freeze ovarian tissue to preserve fertility before undergoing otherwise sterilizing cancer chemotherapy and radiation, and vitrification is preferable to older methods of freezing.
