Successful human ovarian transplantation was first reported with the use of a cortical-tissue grafting technique in monozygotic twins who were discordant for premature ovarian failure.1 Subsequently, six additional cases have been reported, which have resulted in a return of ovulation in all patients, with spontaneous conception and delivery of six healthy infants, with one from tissue that had been frozen.2 The concept of ovarian cortical grafting is based on the fact that all follicles containing eggs are located in the outer 1 mm of the ovary, which can be sutured to the recipient’s medulla just like a full-thickness skin graft. However, a limitation of this technique is that the graft generally loses two thirds of its follicles from ischemia during revascularization, which reduces its life span.3 The patients we have described previously became menopausal after 3 years, although pregnancy then occurred again after grafting of frozen ovarian tissue. Data from studies in animals suggest that microvascular whole-ovary transplantation could avoid this problem.4
A pair of 38-year-old monozygotic twins requested ovary transplantation. One of the sisters had two children and normal ovarian function, whereas the other had undergone premature menopause at the age of 15 years, with amenorrhea for 23 years and a follicle-stimulating hormone (FSH) level of 81 mIU per milliliter.
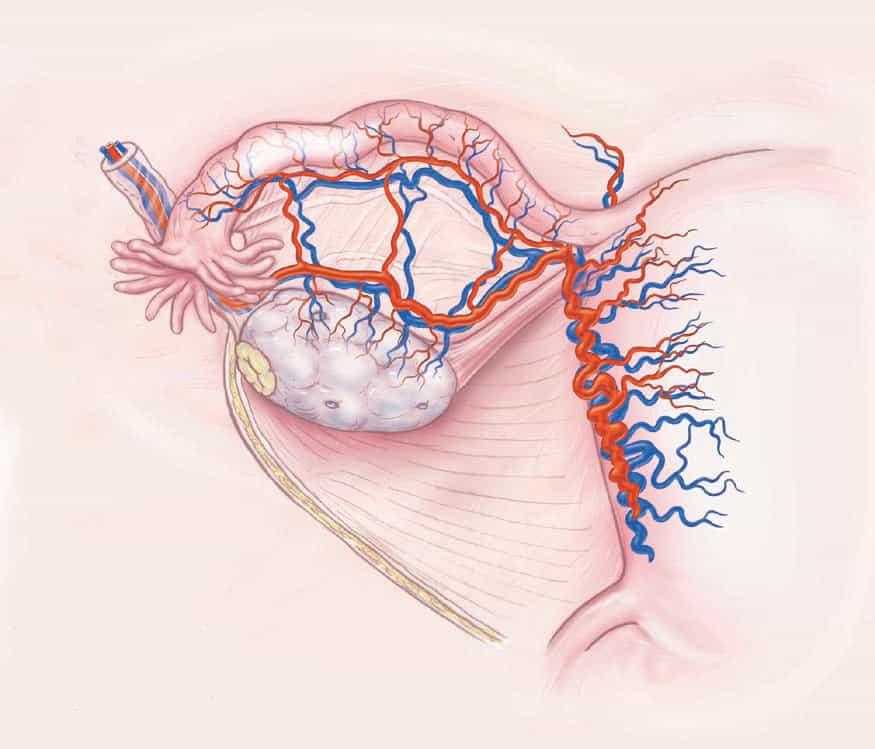
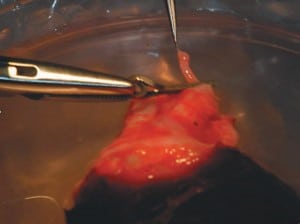
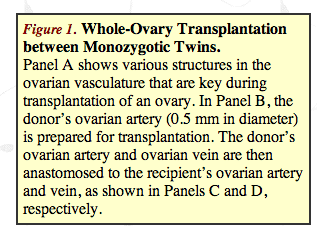
After the procedure was approved by the review board at our institution and written informed consent was obtained from the patients, we laparoscopically removed one ovary from the fertile sister by dividing the infundibulopelvic ligament at its base for maximum length. The ovary was then prepared for microvascular transplantation in the recipient. With the use of minilaparotomy, the donor’s ovarian veins (3.0 mm in diameter) were anastomosed to the recipient’s ovarian veins with 9-0 nylon sutures, and the donor’s ovarian arteries (0.5 mm in diameter) were anastomosed to the recipient’s ovarian arteries with 10-0 nylon interrupted sutures (Fig. 1). Normal-appearing blood flow was immediately observed through the ovarian vessels of the transplanted ovary after an ischemic period of 100 minutes.
The recipient’s first menstruation in 22 years occurred on day 101 after transplantation; by day 158, the FSH level had dropped to 7.4 U per liter. Ultrasonography revealed continuing normal blood flow to the transplanted ovary and normal follicular development. The patient had 11 regular menstrual cycles until, by day 427 after transplantation, the level of beta human chorionic gonadotropin was 174 mIU per milliliter. The results of ultrasonography performed at 7, 10, and 12 weeks for prenatal evaluation were normal. A healthy baby girl was born November 11 at 40 weeks, with an Apgar score of 9/10; the baby weighed 7 lb 15 oz and was 21.25 in. in length. Both mother and baby are doing well. Although technically more challenging than ovarian cortical grafting, whole-ovary microvascular transplantation may result in a longer duration of graft function, although this aspect requires further study. The delay of 101 days until the first menstruation is consistent with the projected time course of follicular growth in humans, since it takes 3 months for eggs in small preantral follicles to reach sufficient maturity to enter the menstrual and ovulatory cycles.5 This case demonstrates the potential for using whole-ovary transplantation between monozygotic twins who are discordant for premature ovarian failure, in order to restore fertility in the affected twin.
Sherman J. Silber, M.D.
St. Luke’s Hospital
St. Louis, MO 63017
Gedis Grudzinskas, M.D.
London Bridge Fertility, Gynaecology, and Genetics Centre
London SE1 9RY, United Kingdom
Roger G. Gosden, Ph.D.
Weill Medical College of Cornell University
New York, NY 10021
- Silber SJ, Lenahan KM, Levine DJ, et al. Ovarian transplantation between monozygotic twins discordant for premature ovarian failure. N Engl J Med 2005;353:58-63.
- Silber SJ, Gosden RG. Ovarian transplantation in a series of monozygotic twins discordant for ovarian failure. N Engl J Med 2007;356:1382-4.
- Donnez J, Martinez-Madrid B, Jadoul P, Van Langendonckt A, Demylle D, Dolmans MM. Ovarian tissue cryopreservation and transplantation: a review. Hum Reprod Update 2006;12: 519-35.
- Wang X, Chen H, Yin H, Kim SS, Tan SL, Gosden RG. Fertility after intact ovary transplantation. Nature 2002;415:385.
- Gougeon A. Dynamics of follicular growth in the human: a model from preliminary results. Hum Reprod 1986;1:81-7.
Image A Image B Image C Image D
See also: