Infertile patients cannot afford to wait for treatment while their eggs get older.
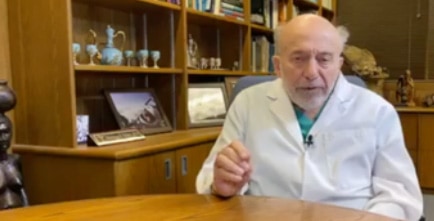
Dr. Sherman Silber, Infertility Center of St. Louis, is offering video consultations for patients who need to plan now for their treatment while stay-at-home orders are in place. He is talking to and evaluating patients in their home to comply with social distancing measures.
Dr. Silber is discovering that patients actually prefer this method of telemedicine consultation over the conventional office visit. Patients have conveyed that “it is so much more convenient and less stressful” to have a telemedicine personal consultation than to take a day off from work to travel to the doctor’s office and sit with other nervous patients in the waiting room.
The COVID-19 pandemic is thus changing much of the way we will do things in the future, and for the better. “Our patients are surprisingly much happier with this approach. Of course, at some point we need to perform hands on treatment. But with this new manner of seeing patients, we can come to the right diagnosis and treatment plan for most patients more efficiently, quickly, and painlessly, with no loss of personal one-on-one communication.” This is a very welcome new era of telemedicine that has been forced on us by the current difficult times.