Rob Stein
E-mail address: silber@infertile.com (Sherman Silber).
NPR, Morning Edition, July 19, 2016
Download the PDF Version of this Article
Dr. Sherman Silber, a renowned pioneer in microsurgery and infertility, is considered one of the world’s leading authorities on IVF, sperm retrieval, ICSI, vasectomy reversal, male infertility, Y chromosome, tubal ligation reversal, egg and embryo freezing, ovary transplantation, and the reproductive biological clock. He performed the world’s first microsurgical vasectomy reversal, as well as the first testicle transplant, in the 70’s and now in the current century, the world’s first ovary transplant. He was the first to develop the TESE and MESA techniques for retrieving testicular and epididymal sperm in azoospermic men. He headed the clinical MIT team that first mapped and sequenced the Y chromosome in infertile men and discovered the now famous DAZ gene for male fertility. His research includes also the study of reproduction and fertility in zoo animals and endangered species. Most recently he has perfected the preservation of fertility for cancer patients with ovarian freezing and transplantation and thereby figured out how to extend the reproductive biological clock of women. He has helped pioneer minimal ovarian stimulation to reduce IVF costs.
When Sarah Gardner was 34, she started getting worried about whether she’d ever have a baby. So she took a test that aims to measure a woman’s fertility.
The results terrified her. They indicated she had the fertility of a woman a decade older — a woman in her mid-40s.
“I was devastated,” Gardner says. The news hit her especially hard because she was in the midst of breaking up with her longtime boyfriend.
“I knew that being a mom was something I wanted in my life,” she says. “And I knew that it would be very difficult to achieve that, given that I was about to be single. So, yeah, I was devastated.”
In her hunt for a solution, Gardner eventually found Dr. Sherman Silber, who runs the Infertility Center of St. Louis. 8 years ago, Gardner discovered, Dr. Silber does something innovative and new for cases like hers — he removes and freezes one of a woman’s ovaries to put their biological clocks on hold.
The idea is that the ovaries can then be thawed and returned to the woman via simple outpatient surgery when they’re ready to try to have children.

Gardner, who lives in Australia, discussed that option with her identical twin sister, Joanne, who lives in London. Joanne was also worried about running out of time to have kids. So both sisters decided to undergo the procedure, as a hedge against their rapidly dwindling fertility odds.
“What it gave us was huge amounts of relief,” Sarah Gardner says. “It really just took a huge weight off us.”
Now, eight years later, the Gardner twins are 44; Sarah just got engaged and wants to finally try to have a baby. She and Joanne both returned to Dr. Silber’s St. Louis office in June to get their ovaries reimplanted.
“It’s weird,” Sarah Gardner says. “It’s like we went in a time machine — a fertility time machine. It’s amazing.”
Not only do the sisters hope their reimplanted ovaries will help them get pregnant, they are also hoping the procedure will reverse their menopause.
“I’m really excited,” Sarah says. “It will be really nice to not have another hot flash.” The approach was originally developed for women being treated for cancer and hope to preserve their fertility but don’t have time to freeze their eggs. Cancer treatments typically destroy fertility.”
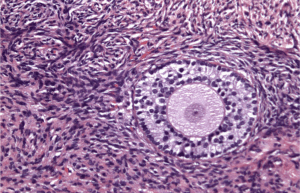
Although removing ovarian tissue (or an entire ovary) and preserving it, then reimplanting it years later has produced promising results for cancer, doing this for non-cancer patients simply to put their biological clock on hold is new. Dr. Silber warns that this is experimental but very promising. The Gardner sisters may be the first women without a history of cancer to have undergone the procedure according to Silber.
Egg freezing, which Dr. Silber also pioneered, has been studied more extensively. Dr. Silber tells patients that egg freezing is far from certain success. While the procedure may seem less invasive, it is more obtrusive, involving often 3 cycles of IVF hormonal stimulation and a huge cost cost compared to ovary tissue freezing.
Silber says freezing, thawing and reimplanting an ovary is easier, more reliable and safer than egg freezing; typically, harvesting the ovary and reimplanting it can both be done on an outpatient basis, he says.
Moreover, when an entire ovary is frozen, women don’t have to undergo the weeks of hormonal injections required to ripen the multiple eggs that are extracted when the eggs are to be frozen, Silber says. And the total cost of the procedure to remove, freeze, thaw and and reimplant and reattach an ovary — less than $3,000 — is much lower, he says, than the $50,000 cost of going through several attempts to collect eggs for freezing.
“There are huge advantages to this,” Silber says. Meanwhile, the Gardner sisters are once again home in Australia and England. They’re both waiting for their periods to start again and hope to be pregnant by the end of the year.
“Wouldn’t that be nice?” Sarah Gardner says, adding that she and her sister realize that the doctors can’t guarantee success.
“We’re going to leave it up to the gods or the universe,” she says, “and see what happens.”
Correction July 19, 2016: An earlier headline on this story said that the Gardner sisters had ovaries removed and frozen in 2012. They actually had the procedures in 2009.
Citation – Portions of this article were featured on NPR’s Morning Edition July 19, 2016.
Rob Stein “Twin Sisters Try to Get Pregnant with Ovaries They Froze in 2009.” Morning Edition National Public Radio, July 19, 2016. https://www.npr.org/sections/health-shots/2016/07/19/485838529/twin-sisters-try-to-get-pregnant-with-ovaries-they-froze-in-2009
Download the PDF Version of this Article
See also:
