Dr. Silber Explains Male Infertility on Netflix
Low Sperm Count/Oligospermia
For men with a low sperm count or Oligospermia, there are no additional treatments or surgeries needed because we use ICSI with every case.
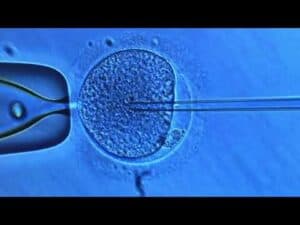
ICSI (Intra Cytoplasmic Sperm Injection)
If there is a question of the sperm’s ability to fertilize the egg, due to either a low sperm count or poor quality of the sperm, that poses no problem whatsoever. Intra-Cytoplasmic Sperm Injection (ICSI) would be performed instead of regular In vitro fertilization (IVF). With ICSI, the eggs are retrieved the same as if you were doing conventional IVF. However, the eggs and the sperm are then fertilized in the laboratory, by direct injection of a single sperm into each egg. Three days later the resulting embryos are simply placed into your uterus with no surgery, just as with IVF. Extra embryos are frozen for later attempts at pregnancy.
Azoospermia
There are many infertile couples in whom the male is completely azoospermic (that is, no sperm at all in the ejaculate). For these cases, the urologist is actually needed, but again, often, his treatment is poorly performed.
There are two entirely different situations and causes for no sperm in the ejaculate (azoospermia): obstructive and non-obstructive. For obstructive azoospermia, aside from vasectomy, which is reversible with reconstructive microsurgery, there are men who were born with the absence of the vas. Most of them have a mutation on their CF (cystic fibrosis) gene or chromosome 7 but do not have cystic fibrosis. They just never developed a vas deferens in fetal life, and they do not discover they have this problem until they get married, try to have children, and discover they have no sperm in the ejaculate. There are no vas deferens to reconstruct so the only way they can have children is to microsurgically retrieve sperm from their epididymis and inject this sperm into the wife’s eggs via IVF. This procedure is virtually 100% successful.
Sperm Aspiration
Men with no sperm at all in their ejaculate can now have their own child, because sperm can be retrieved from their testicle or epididymis and injected into their wives’ eggs. The highest pregnancy rates with this approach and the least pain and discomfort to the male require that these sperm retrieval procedures be performed microsurgically, and not with either crude needlesticks or gross surgical techniques.
Even when there is no sperm whatsoever in the man’s ejaculate (azoospermia), there is now a very good chance for pregnancy using our sperm retrieval and ICSI procedures. The techniques of sperm retrieval and ICSI were originally developed by us in Brussels, Belgium, and in St. Louis, Missouri.
Technical Scientific Talks by Dr. Silber
TESE for Azoospermic Men
Men with non-obstructive azoospermia caused by germinal failure can now be treated successfully in many cases using testicular sperm extraction (TESE–a term which we coined in 1993) and ICSI. There is a threshold of quantitative sperm production in the deficient testis, below which no sperm will reach the ejaculate (azoospermia). This threshold phenomenon of spermatogenesis is the reason that many cases of non-obstructive azoospermia, sperm can often be extracted from testicular tissue of azoospermic men with germinal failure, and used successfully for ICSI. A prior diagnostic testicle biopsy analyzed quantitatively can often predict the likelihood of finding such sperm during a TESE-ICSI attempt.
Vasectomy Reversal
It is important to realize that the testicles and the scrotum are a very private and sensitive area for most men. You don’t want to have a compromised procedure on that area of the body performed in the “procedure room” of an office-based clinic, rather than in a proper operating room of a high-quality hospital.
As you will read on the Vasectomy Reversal page, our success rate is over 95% because of our ability to repair epididymal damage, which makes a success with most urologists only about 15%. In addition, there is virtually no pain post-operatively because of the long-acting local anesthetic which we inject. This special anesthetic combination will last for three days after which most of the pain you would otherwise have had will be gone.
Y-Chromosome
Along with the development of ICSI in 1993, our center was the first to study the Y chromosome and male infertility, and why tiny amounts of sperm are often found in the testes of azoospermic men previously thought to be making no sperm. You have probably heard a lot about the Y chromosome. It is what determines that a male is a male. We discovered with our first scientific paper on this in 1995 that the Y chromosome contains many genes that are involved in spermatogenesis, and deletions involving these genes are often found in infertile males.
There has been a great deal of unknowledgeable discussion about our discovery of these sperm producing genes on the Y and a lot of misinformation. So in this page, I will try to clear up the confusion so you will understand better the genetics of male infertility. Our sequencing the DNA of the Y gives us a deep perspective about infertility genes that are widespread throughout the genome and which are also involved in transmitting infertility to future generations. A benefit of understanding the Y chromosome is it will help us to comprehend why men who are seemingly azoospermic usually have some residual tiny amount of spermatogenesis that can be used for successful ICSI. More importantly, it will expose the futility of trying to increase sperm count with drugs or varicocoele surgery.
Male infertility treatment, short of IVF and ICSI, should be limited to microsurgery for azoospermia, and careful thought has to go into making your choice of where to go for such treatment.








 3-300×225-1.jpg 300w, https://www.infertile.com/wp-content/uploads/2024/11/hqdefault-3-300×225-1.jpg 480w”>
3-300×225-1.jpg 300w, https://www.infertile.com/wp-content/uploads/2024/11/hqdefault-3-300×225-1.jpg 480w”>