Dr. Silber Explains Treatment for No Sperm
What Is Azoospermia?
Four million American couples suffer from infertility, and in almost half of those cases, the problem involves a low sperm count in the male. In about 2 percent of these cases, there is no sperm whatsoever, that is, azoospermia.
What Causes Azoospermia?
Azoospermia can be caused either , by obstruction, as in a vasectomy case, or by deficient or no sperm production in the testicles. The most common cause of obstruction is failure of vasectomy reversal, either at the site of reconnection of the vas, or because of blowouts in the epididymis. Most commonly, when performing a vasectomy reversal, physicians who are not extremely comfortable with microsurgery will simply reconnect the two ends of the vas (vasovasostomy) regardless of whether there is blockage from blowouts in the epididymis.
This simple reconnection of the vas will not result in success in at least 80 percent of cases because of this additional blockage in the epididymis. Failure to bypass this epididymal blockage will guarantee failure in the majority of surgeries attempting to reverse vasectomy. We can either re-reverse the vasectomy or retrieve sperm from the obstructed testicle using ICSI, and that sperm can fertilize the wife’s egg.
Azoospermia can also be caused (in the absence of obstruction) by deficient sperm production in the testicles.
How Is Azoospermia Treated?
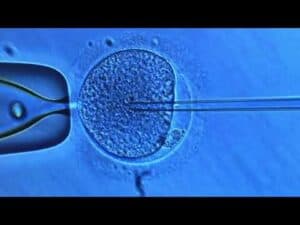
If obstruction is the problem it can often be fixed with microsurgery, but not always. In that case sperm can be retrieved microsurgically and used for ICSI. In fact, we originally invented the procedure mostly for congenital absence of the vas (CBAVD).
A whole variety of ineffective treatments were designed to try to raise the sperm count, but these treatments were all destined to fail because the sperm count is genetically determined in each man and cannot be affected by any of these foolish therapies. For deficient sperm production the only treatment is ICSI. All other treatment to try and raise the sperm count are doomed to fail. Even if there is no sperm at all because of deficient sperm production, we can still retrieve sperm from the testicle and use to get the wife pregnant.
In fact, we invented this procedure.
Dr. Silber is world leader & pioneer of the most widely used in vitro fertilization techniques. His patients fly in long from distances all over the world for treatment at his fertility center and, he is happy to take care of the most difficult cases with warm personal attention and great technical skill.

I remember a twenty-seven-year-old man with sperm count reports that consistently read “only an occasional weakly motile sperm.” The patient had been declared absolutely sterile by a urologist, who had performed varicocelectomy, treated him with Clomid, then Pergonal, then testosterone rebound, and then even made him put ice around his scrotum to cool off the testicles every evening before he went to sleep – or tried to go to sleep. Obviously, none of these foolish treatments improved the sperm count. In the first ICSI cycle we performed for him, his wife became pregnant and delivered healthy twins. His previous doctors had hoped that with all kinds of conventional and ineffective treatments they could make him produce normal, mature sperm. But that was, of course, impossible.
A potentially disastrous case resulting from inappropriate treatment of the male involved a patient who was a prominent doctor from another city. His sperm count was twenty million per cc with 40 percent motility (not really all that bad), but he was told by the chief of urology at a university hospital that his sperm count was not high enough and that he needed a bilateral varicocelectomy. Following his stupid bilateral varicocelectomy, the sperm count went down to zero, and one of his testicles completely disappeared. Obviously, the spermatic artery had been damaged in both cases. The remaining testicle had severe damage, but luckily recovered enough eventually to give him two to five sperm in the ejaculate. This extraordinarily low count, which many would consider the equivalent of zero, was fortunately more than enough for him to be able to get his wife pregnant with an ICSI procedure at our center in St. Louis. Click here to read much more
Azoospermia and Vasectomy Reversal
However, there are many infertile couples in whom the male is completely azoospermic (that is, no sperm at all in the ejaculate). For these cases, the urologist is actually needed, but again often his treatment is poorly performed. For example, I recently saw a couple from Texas that needed a vasectomy reversal procedure. He had had a vasectomy in the past, and needed a reversal to try to have another child. He went to a urologist in Texas who offers “money back” guarantees. I have re-operated on many of the patients of this doctor who failed reversal attempts and I know that none of them ever had their money returned as he always had room in his “contract” to wiggle out.
The doctor he saw lied to him on three counts. Firstly, he told him post-op after the vasectomy reversal that he now had sperm in his ejaculate and that the vas reconnection had been successful. But there was no sperm in the ejaculate, and when we did his re-operation a year later, we found that the two cut ends of the vas were nowhere near each other. Therefore he could never ever have had sperm in his ejaculate after his previous surgery. The second lie was that the doctor said he had found sperm in the vas fluid when he did the vas reconnection. But there were epididymal blowouts indicating there could not have possibly been sperm in the vas fluid. The third lie was that he could possibly have had a successful reversal even if a vas reconnection had been performed, because what he needed was a reconnection of the vas to the epididymis proximal to the blowout site.
So taking all three of these lies into account, we re-operated on this patient who supposedly had had a successful vasectomy reversal back home in Texas, doing a rather extensive procedure to free up all the surgically induced scar tissue, and reconnected the vas to the epididymis on both sides. Now he truly is fertile, with normal sperm count, and has successfully impregnated his wife finally, with no need for IVF.
Azoospermia Not Caused by Vasectomy
Obstructive Azoospermia
If the azoospermia is not caused by a previous vasectomy, it is usually not correctable with reconstruction, and then sperm with IVF and ICSI is necessary. In fact, we were the center that invented sperm retrieval with ICSI or azoospermic men in the 1990s, and have the greatest experience and expertise with it.
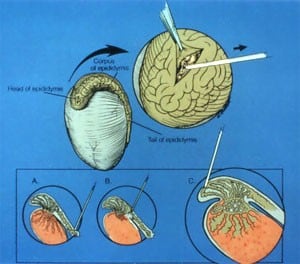
There are two entirely different situations and causes for no sperm in the ejaculate (azoospermia): obstructive and non-obstructive. For obstructive azoospermia, aside from vasectomy, which is reversible with reconstructive microsurgery, there are men who were born with absence of the vas. Most of them have a mutation on their CF (cystic fibrosis) gene or chromosome 7, but do not have cystic fibrosis. They just never developed a vas deferens in fetal life, and they do not discover they have this problem until they get married, try to have children, and discover they have no sperm in the ejaculate. There is no vas to reconstruct and so the only way they can have children is to microsurgically retrieve sperm from their epididymis and inject this sperm into the wife’s eggs via IVF. This procedure is virtually 100% successful.
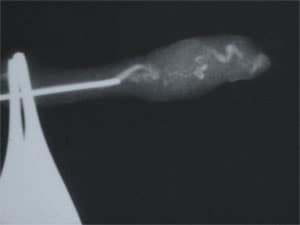
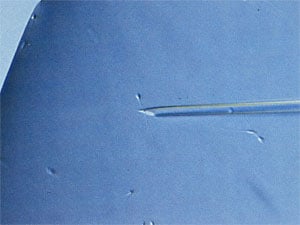
In both types of sperm retrieval, obstructive and non-obstructive, it is important to use precise microsurgical techniques rather than just “needle sticks” to have the highest percentage of success and also the least amount of pain or complications. Unfortunately, this is not always the case, and some husbands have fairly horrible experiences, which just shouldn’t happen. For example, I just recently saw a couple who had gone through 10 IVF cycles with retrieval sperm for congenital absence of the vas at a reputable IVF clinic, with over 20 embryos transferred but no pregnancy. Each time he had the sperm retrieval done with a needle stick rather than microsurgery, and each time relatively poor quality sperm were used because the urologist could not see where in the epididymis he was poking. So he retrieved mostly older sperm with a lot of DNA fragmentation, thus explaining the wife’s failure to conceive. Furthermore, he had a great deal of pain and swelling with each crude needle stick procedure making his wife frustrated when he became less and less enthusiastic with each IVF cycle at the thought of going through another one. Also, the sperm the urologist had retrieved was so poor that the laboratory would not freeze it, even though the proper approach would have been to obtain good quality sperm that would freeze well and obviate any further need for sperm retrieval.
There are countless cases I have seen of this kind of mismanagement of male infertility at office IVF centers that have no microsurgical knowledge of the male. Just recently we saw an azoospermic patient who had been diagnosed at 10 years of age with a rare condition called Kartagener’s Syndrome, where their ciliated cells in the lungs and nose and even the epididymis (the tiny duct which carries sperm out of the testicle into the vas deferens) are unable to move. The tiny hair-like cilia can’t wiggle and sweep the fluids along well, but modern treatment makes it a minor condition except for one thing: they have no sperm in the ejaculate.
This patient wasted years of time, energy, and money going through worthless testing, while his wife’s eggs were getting older. When he finally reached our clinic, the same day I performed a microsurgical sperm retrieval under local anesthesia, which resulted in our obtaining millions of vigorous motile sperm perfect for IVF. His previous clinic had thought that his Kartagener’s Syndrome would make his sperm non-motile and nonfunctional even for VF, but clearly that was not the case. The sperm were perfectly normal. They just couldn’t get out of his epididymis into the ejaculate.
Non-obstructive Azoospermia
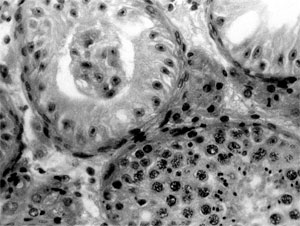
The second type of azoospermia is “non-obstructive.” This means there is not any obstruction, but the patient “appears” to have just no sperm production at all in his testes. Usually this is partly just an illusion, in that the majority of such patients do have a tiny amount of sperm production in their testes, but just not quantitatively enough sperm production to “spill over” into the ejaculate. These cases should usually, but not always, be successful in retrieving enough sperm for successful IVF and ICSI.
Another recent example of the poor quality of male infertility treatment at many IVF clinics I saw recently was even more tragic than what I have already described. This was a patient with non-obstructive azoospermia who was sent by his clinic to a urologist who did a useless varicocele operation on both sides in a highly scarred and difficult inguinal area, because the cause of the azoospermia was undescended testis, as well as very destructive testis biopsy on both sides. The result was that in addition to azoospermia, he now also had no testosterone production either. This poor patient became a eunuch as a result of the overzealous and poorly performed attempt at sperm retrieval he had to suffer through.
Klinefelter’s
A good example of the one of the most difficult cases of azoospermia is the so-called Klinefelter’s in which the azoospermic man has two X (47XXY) chromosomes instead of one X (46XY) chromosome. It used to be thought that these men could never father children and had the worst prognosis of any male infertility. In truth, most of these cases have been successful in our hands.
Despite very tiny testicles, these men usually have adequate, though modest, testosterone production, and shockingly we can usually find enough sperm in these tiny testicles for them to father children via ICSI. But great care must be taken in this type of microsurgery to preserve their very reduced but adequate testicular function.
Why TESE is less harmful than Microdissection
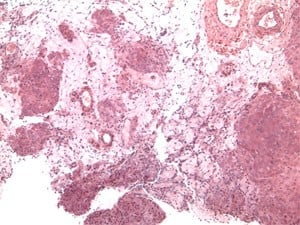
Unfortunately, most urologists today have been taught to use the disastrous Schlegel technique of microdissection. This Schlegel operation advertises that it does less damage to the testes, and this is totally false. The opposite is true. Most patients after the Schlegel microdissection are eunuchs after this procedure. It digs deep into the testicle and destroys blood supply. Unfortunately, urologists are taught to do this only because Dr. Schlegel is such a convincing charlatan.
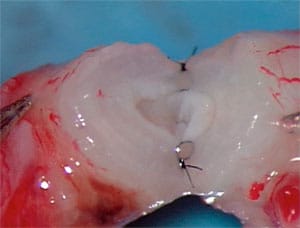
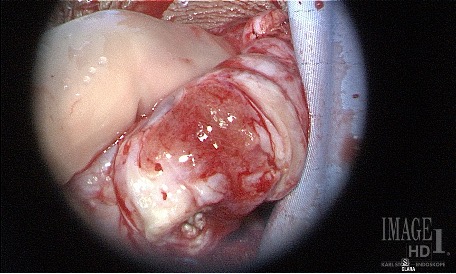
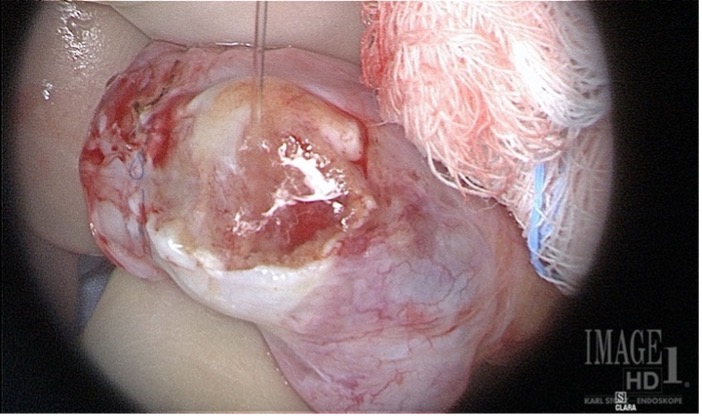
Tragically these pictures below are examples of two cases we just saw who had the Schlegel procedure a year ago and you can see that two-thirds of their testicles were destroyed and converted to scar tissue.
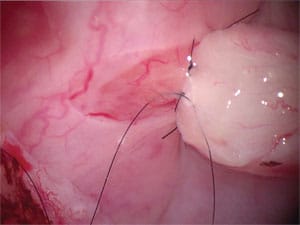
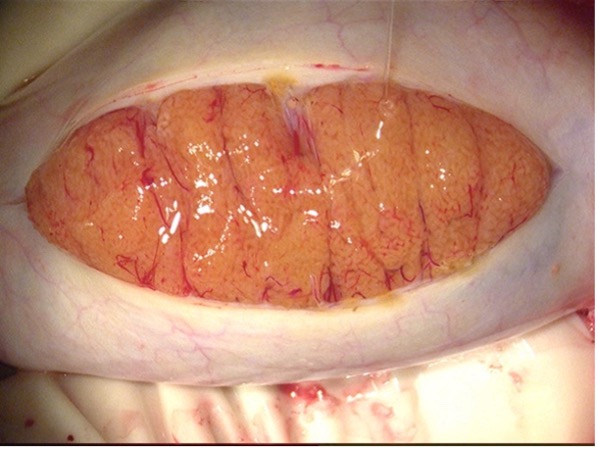
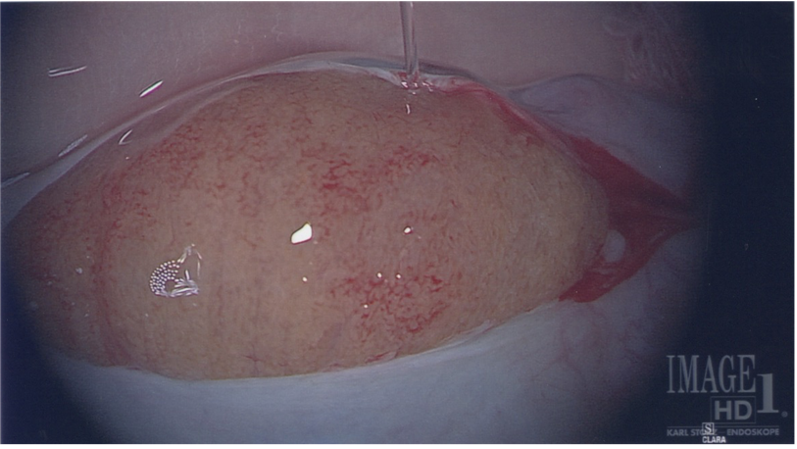
These pictures below show how the testis should look after a TESE proceedure.
If you have any questions, you may call us at (314) 576-1400.