Dr. Silber Explains

It is important to realize that the testicles and the scrotum are a very private and sensitive area for most men. You don’t want to have a compromised procedure on that area of the body performed in the “procedure room” of an office-based clinic, rather than in a proper operating room of a high-quality hospital.
As you will read in the details below, our success rate is over 95% because of our ability to repair epididymal damage, which makes a success with most urologists only about 15%. In addition, there is virtually no pain post-operatively because of the long-acting local anesthetic which we inject. This special anesthetic combination will last for three days after which most of the pain you would otherwise have had will be gone.
It is sad to see patients spend $6,000 to $10,000 on a botched attempt at vasectomy reversal elsewhere in a too simple outpatient procedure room, where they had little chance for success, and yet suffered enormous pain and swelling, completely unnecessarily. Of course, we can fix the mess created by a previous botched reversal attempt, but it is a shame not to have had it done correctly in the first place in a proper hospital operating room. Patients who come here to fix their previously botched surgery often tell horror stories of how they were sent back home, or to their hotel, right after surgery with pain and swelling and no drains. From their surgery here they have very little pain or swelling, and much more rapid healing, because of our more comfortable overnight inpatient approach. With a new local anesthetic that we are using for our microsurgical procedures at the time of incision closure, patients are experiencing virtually no postoperative pain following surgery. The effect lasts for a full three days, and by then there is normally hardly any pain anyway. This means virtually no pain from tubal reversals, vasectomy reversals, ovary transplants, or myomectomies, or even just MESA or TESE sperm retrieval procedures. So your pain now postoperatively at worst from the most major procedures may require very little medication,
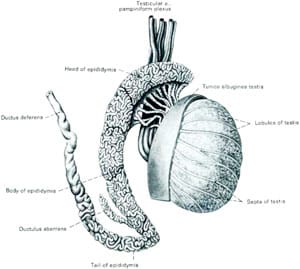
Vasectomy Reversal is a procedure (first invented and reported by Dr. Sherman Silber in 1975) which allows men who have previously undergone a vasectomy to become fertile again. The vas deferens is microsurgically reconnected and the epididymal blowouts are microsurgically bypassed, allowing sperm to travel out of the epididymis and into the ejaculate. In 85% of vasectomy patients blowouts are found in the epididymis. So failure to correct or bypass these blowouts leads to poor success rates. But with proper attention to these details over 95% of men have a return of fertility.
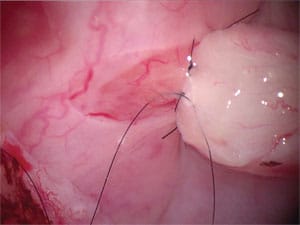
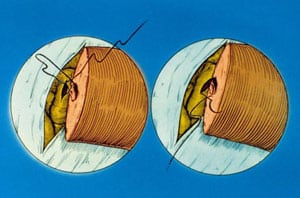
Microsurgical Vasectomy Reversal Technique For Simpler Cases (15% of cases)
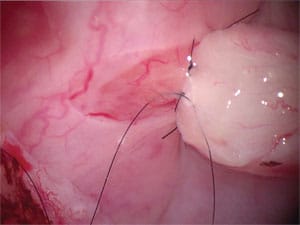
The outer diameter of the vas deferens (sperm duct) is about 1/8 of an inch, but the diameter of the inner canal which carries the sperm is about 1/70 to 1/100 of an inch or roughly the size of a pinpoint. This inner canal has a lining of mucosa which is about 3 cells thick. In order to achieve a non-obstructed reconnection, it is necessary to accurately stitch this inner lining in a leakproof fashion, using thread that is invisible to the naked eye (approximately 1/1000 of an inch in diameter). Then the relatively thick muscular wall (1/16 of an inch on each side) is similarly stitched to insure proper muscular contraction for moving sperm into the ejaculate.
This is all performed under a microscope with very high magnification, using delicate instruments and suture which I designed specifically for this surgery.
There are less precise techniques for vasectomy reversal. For example, a single-layer of stitching that pierces through the thicker muscular wall and the delicate inner lining all in one bite will not obtain as precise an approximation and runs the risk of actually sewing the tiny inner canal shut.
In most cases, attempting to reverse the vasectomy simply with “vasovasostomy” or “vas-to-vas reconnection” is simply not adequate because, over a period of time, blockages occur in the epididymis, i.e. closer to the testicle. This epididymal damage must be bypassed and is much more difficult microsurgically than simply reconnecting the vas.
Vasectomy Reversal Pitfalls
There are many traps to watch out for when choosing a doctor to perform your reversal.
For example, some doctors will offer a “money-back guarantee,” but patients rarely get their money back after a failed procedure despite promises to the contrary.
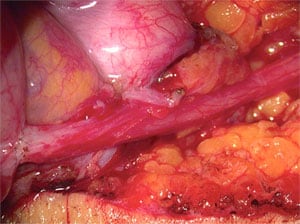
![Precise microsurgical alignment of the inner canal of the vas lining with ultra-fine monofilament surgical thread that is invisible to the naked eye performed under the microscope with high powered magnification usually results in a normal channel for sperm to travel through and gives the best chance for a pregnancy. [Watch video]](https://www.infertile.com/wp-content/uploads/2014/11/Microsurgical-allignment.jpg)
We have operated on many patients whose previous vasectomy reversal attempts at “money-back guarantee centers” had failed, and none of these patients have ever gotten their money back. There was always some fine print wording that allowed the clinic to keep their money despite the “money-back guarantee.”
In most so-called “centers,” the only procedure performed to reverse the vasectomy is “vasovasostomy” to try to reconnect the severed vas. However, in most cases, there is also “epididymal” blockage (closer to the testicles) created by the pressure build-up after vasectomy. Thus, there is no chance for most cases of “vasovasostomy” to be a success, because there is also a blockage in the more delicate duct closer to the testis, and this would have to be bypassed also with a very tricky-to-perform“vasoepididymostomy” [technical video] in order to have a successful result.
Another trap is that these less successful commercial operations are always performed at little outpatient centers or clinics, and not at a major hospital like St. Luke’s Hospital in St. Louis. Therefore, the patient is sent home, or to his hotel room, only a few hours after his operation. The natural consequence is often a huge amount of pain and swelling, and several miserable months of post-operative recovery. We think it is imperative for the patient to stay overnight for one night in the hospital, with drains in place and nurses changing the dressings, which prevents pain and swelling and results in a faster and much more pleasant post-operative recovery. When we “redo” a messed up “vasovasostomy” done elsewhere that had failed, despite it being a bigger operation to bypass all the scar tissue created by the previous failure, our patients are elated by how little pain and swelling they had to endure compared to their original failed reversal surgery in an outpatient office or clinic setting.
In fact, the only reason to do this operation in such an office or clinic setting is to save on overhead and make more money on the procedure. We do not condone this common practice. Furthermore, if the cost is the important issue (and it is for many people), it is far less cost-effective to have a “vasovasostomy” that fails, with significant pain and swelling afterward, than to just do it right in the proper hospital setting the first time.
The next big trap is that clinics that cannot perform the delicate microsurgery required, will suggest you do sperm retrieval and IVF (in vitro fertilization) instead of vasectomy reversal. We have nothing against sperm retrieval and IVF since it is our center that actually invented it in 1987, over 20 years ago. However, we invented it as a second choice approach for those in whom a reversal was not possible because of a complete absence of the vas deferens. Otherwise, it is so much nicer just to have one operation that restores your original fertility, without your wife having to go through months and months of painful injections involved in IVF, with a pregnancy rate lower than what you would achieve through natural intercourse once you have had a successful reversal.
Finally, it is important to realize that the testicles and the scrotum are a very private and sensitive area for most men. You don’t want to have a compromised procedure on that area of the body performed in the “procedure room” of an office-based clinic, rather than in a proper operating room of a high-quality hospital.
Failure Of Previous Reversal Attempts
The technique is equally successful in cases where previous attempts at vasectomy reversal elsewhere have failed. In these circumstances, scar tissue from the previous operation does make repeat surgery more difficult, but that poses no problem with results. In my experience, previous failed surgery has never interfered with obtaining an accurate reconnection. I do not recommend that you go through the expense and discomfort of a less meticulous attempt at vasectomy reversal the first time. Nonetheless, if you have had a previous unsuccessful operation elsewhere this will not hurt your chances for success if you come here for a repeat operation.
In fact, 40% of my patients come here after having had a failure of a vasectomy reversal attempt elsewhere. The cause of these failures is always obstruction. In many cases, obstruction is at the site of the previously attempted reconnection. However, in most patients, there is also obstruction in the much more delicate ductwork closer to the testicle, called the “epididymis.”
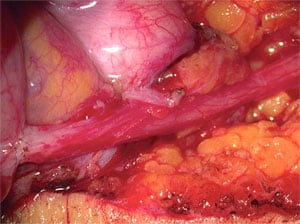
The Need For Epididymal Repair (More Complex Cases)
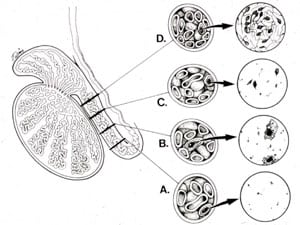
The epididymis is a coiled, 20-foot long, fragile, microscopic tubule that carries sperm from the testicle into the vas deferens. The delicate wall of this tubule is a thin, filmy membrane 1/1000 of an inch in thickness. The diameter of the tubule is 1/300 of an inch, or roughly 1/3 the size of a pinpoint. After the vasectomy, the testicle continues to produce sperm and fluid normally. This causes a build-up of pressure within the vas going all the way back to the epididymis. In most individuals, this pressure causes a “blowout” in the epididymis, similar to a leak in the thinnest part of a tire that has more pressure than it can handle. The sperm then leaks into the surrounding tissue and causes scarring and obstruction.
Thus the patient has obstruction not only at the original vasectomy site but also closer to the testicle, at the epididymis’ blowout site. In this situation, reconnection of the vas deferens alone would not restore fertility. Such patients require a more precise reconnection of the vas deferens to this much more delicate epididymis.
The majority of vasectomized men have such epididymal blowouts. The longer the duration of time since your vasectomy, the greater the chance that you will have epididymal obstruction. However, it is important to understand that epididymal blow-outs can occur anytime following your vasectomy. If this has happened to you, these blow-outs will need to be repaired at the time of your reversal to maximize your chance of regaining fertility.
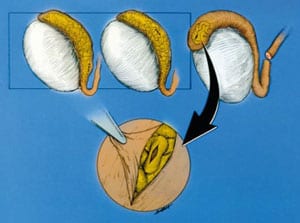
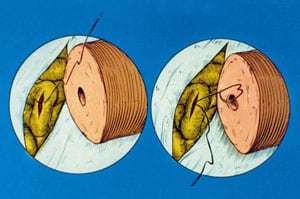
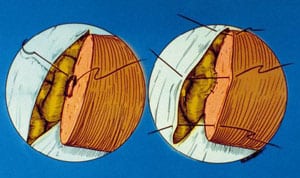
Microsurgical Vasectomy Reversal Is Not Just Vasovasostomy
Vasectomy reversal is often incorrectly thought of as simply a reconnection of the severed vas deferens. In fact, the term many doctors mistakenly use for the reversal of vasectomy is “vasovasostomy”. But vasovasostomy just means reconnecting the vas. Simply “reconnecting the vas” is not enough to restore fertility to most vasectomized men. The reason for so many failures of vasectomy reversal, even with “microsurgery”, is that in over 80 per cent of cases the pressure buildup inside the vas (caused by the original vasectomy) results in microscopic “blowouts” and “concretions” in the more delicate ductwork closer to the testicle (called the “epididymis”) which is where the sperm leave the testis on their way to the vas. If this complex, truly more delicate pathway, the epididymis, is not microscopically bypassed, the vasovasostomy will not work, because the sperm still cannot get to the site of the vas reconnection. They are blocked from even reaching the vasovasostomy site because the more delicate ductwork closer to the testicle remains blocked. So the routinely performed vasovasostomy was destined never to work no matter how accurate the reconnection.
The reason for this most commonly practiced error is that repair of the epididymis is very difficult, and requires years of very specialized practice and experience. Most urologists would be lost in the epididymis. So they might very earnestly apply what they think are “microsurgical skills” to perform a vasovasostomy, just hoping that there are no proximal blowouts in the epididymis. They might even tell the patient that they saw “sperm” in the vas fluid at the time of the vasovasostomy, increasing their hope that vasovasostomy is enough in their case. They will do anything to avoid trying to repair the usually obstructed epididymis because it is so difficult for the less experienced.
The problem is that there will always be creamy thick fluid in the vas deference on the proximal side of the vasectomy site, which has been stored in that obstructed site for years, and there might even be decayed old dead sperm or sperm parts in that fluid, and so it might be mistaken for epididymal continuity. But if the vas does not have translucent fluid with normal intact motile sperm, then you can be sure that no fresh new sperm has reached this area for many years, because of epididymal blockage more proximally. So you might leave the clinic with “wait and see” advice from the doctor even though there is no chance of the “vasovasostomy” working. It may not be until a year later with consistently negative semen analysis results, that you realize you had the wrong operation.
This problem of epididymal blowouts is much more common now than 20 or 30 years ago, and occurs much earlier after vasectomy, as early as 6 months even. The reason is that urologists are performing the original vasectomy much more tightly, allowing no leaks whatsoever of sperm. Therefore, it is important for the microsurgeon to perform this more delicate vasoepididymostomy procedure [technical video] in over 80 percent of cases when there is a secondary epididymal blockage.
Poor Sperm Counts After Less Precisely Performed Vasectomy Reversal
Sometimes patients may think they have had a successful vasectomy reversal because there is some sperm in the ejaculate, but the sperm count is terribly low and they are not really fertile. With imprecise surgery an adequate channel is not established, scarring constricts the site of reconnection, impeding sperm transport, and this causes the sperm count to be too low. Also, unrepaired epididymal damage reduces the quality and quantity of sperm getting through. Pregnancy is not likely with that sort of result.
Large Segment of Vas Removed At The Time Of The Original Vasectomy
The length of vas removed at the time of vasectomy and the type of vasectomy originally performed should not have any effect on the results. Whether or not the convoluted portion of the vas is involved is of no consequence. The vas can be microscopically stitched just as precisely in the convoluted as in the straight portion. If a large segment of vas has been removed, the gap can always be bridged by careful microsurgical dissection.
It is impossible to determine prior to surgery just how much vas deferens was removed at the time of your vasectomy. It is never an important concern. The success rate should not be any lower in cases where large or even huge portions of the vas have been removed.
Difficulty Of Operation
This surgery requires a great deal of practice, because of the delicate manipulations involved. I practiced on over 2,000 rats for three years before performing my first human case. I have now performed over 7,000 cases and close to 14,000 microsurgical reconnections on humans. I do not recommend this procedure to be tried on humans without adequate and continuing practice.
In addition to enhancing the likelihood of success, performing this surgery delicately allows there to be less pain and swelling postoperatively, with a quicker and more comfortable recovery. In fact, the pain postoperatively should be minor IF proper attention is paid to all these details.
Infertile couples from all over the world come to St. Louis, Missouri, to chase their dream, because Dr. Sherman Silber and his team are simply the best there is.
Discovery Health Channel Documentary

Fertility And Pregnancy Results
The statistics reported in this information are based strictly on surgeries performed by myself on over 6,000 patients and do not reflect the results of other surgeons. These statistics are not estimates or guesses, but represent an accurate tabulation of the results in those patients I have already operated on.
- 98% of patients develop normal sperm count and sperm motility, indicating fertility. 88% achieve pregnancy without further treatment.
- Contrary to general myth, the duration of time since vasectomy does not significantly affect the success rate.
- The success rate for those patients who have had previous unsuccessful surgery elsewhere and come here for a re-operation is no different from patients who are undergoing vasectomy reversal here for the first time.
- We always freeze sperm retrieval at the time of surgery, so that the 2% who are failures will have sperm available for IVF just in case the reversal turns out not to be successful.
Cost-Effectiveness of Vasectomy Reversal Compared To Sperm Retrieval With ICSI
- The cost of sperm retrieval and ICSI is much higher than for vasectomy reversal, but the pregnancy rate after a single microsurgical vasectomy reversal is over 80%, and with ICSI is about 40% per treatment cycle.
- Therefore the first choice is vasectomy reversal. Sperm retrieval and ICSI is only a “back up”, which hopefully won’t be needed.
If you have any questions, you may call us at (314) 576-1400.
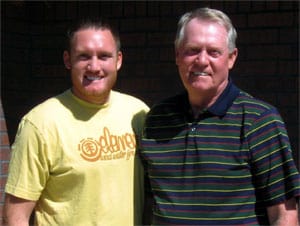
Father and Son Story
Comment from Dr. Silber:
Todd, left, is a young man who was born after I did a vasectomy reversal on his father, right, 31 years ago. 31 years later, at age 31 I also did a vasectomy reversal on his son, Todd. Both were successful, both on father and on son 31 years later. So maybe we will be seeing his son 31 years from now.
Follow up note from Dr. Silber:
Todd is overjoyed because his wife became pregnant 3 months after his vasectomy reversal and emphasized that he would not exist if Dr. Silber hadn’t operated on his father 30 years before, and his baby would not exist now if Dr. Silber hadn’t operated on him. 3 generations of Silber children!
Todd Damron
Honolulu, HI