Dr. Silber Explains
Click Here to Learn More about Tubal Reversal Cost and How to Arrange for Surgery.
Click Here to Learn More about Tubal Ligation from Chapter 15 of Dr. Silber’s book, “How to Get Pregnant“.
A common dilemma many individuals face if they’ve previously had a tubal ligation is whether they should undergo a microscopic tubal ligation reversal vs. an In Vitro Fertilization (IVF) procedure. While a tubal reversal does require more skill than an IVF procedure, a tubal reversal is actually the better option for most patients. A tubal reversal requires one operation to restore fertility, enabling the patient to have as many children as she wants, whereas an IVF procedure offers a lower, 20% to 35% chance of success for each try and can be much more costly in that it could take several attempts before becoming pregnant. Our success rate with microsurgical tubal reversal is about 95%. (We actually were the first to develop this procedure in the U.S., and therefore have the largest experience with it now in the world.) The procedure involves a relatively small incision and only one day in the hospital. There is very little pain, and you can go back to work within a week. With a new FDA approved local anesthetic that we are using for our microsurgical procedures at the time of incision closure, patients are experiencing virtually no post operative pain following surgery. The effect lasts for a full four days, and by then there is normally hardly any pain anyway. This means virtually no pain from tubal reversals, vasectomy reversals, ovary transplants, or myomectomies, or even just MESA or TESE sperm retrieval procedures. So your pain now post operatively at worst from the most major procedures may require just Extra Strength Tylenol.
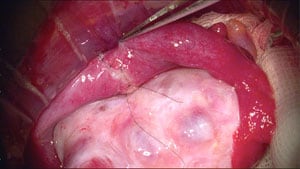
The fallopian tube is a tiny passageway that begins at the fimbrial end where the egg is picked up from the surface of the ovary, and leads through a microscopic opening into the uterus. As long as the fimbrial end has not been destroyed we can achieve an excellent micro-anatomical reconnection.
If a large amount of tube was destroyed by your original sterilization, that will not interfere with our achieving an accurate surgical re-connection. However, your chance for pregnancy is related to the length of the tube. If at least one-half of the tube is still intact, the chances for pregnancy will be over 90%. If there is a shorter length of tube, the chances for pregnancy will be less. As the amount of tubal length diminishes, the chance of pregnancy diminishes despite an accurate re-connection. Pregnancy can never be promised. However, a good microscopic operation is necessary to give you the best chance of restoring your fertility.
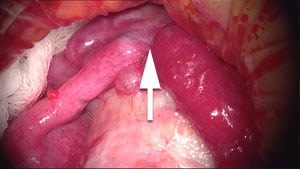
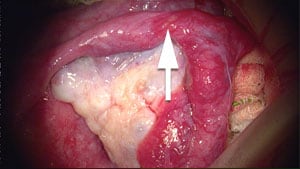
The diameter of the tube varies in different sections. Because your tubal sterilization has destroyed a certain segment of your tube, the two ends which to be reconnected will most probably be of different size. Through the use of microsurgery we can beautifully reconnect these ends of the tube even when there is a difference in size. It is technically possible to connect the relatively large diameter near the fimbriated end to the tiny almost invisible cornual end. However, it is important to microscopically tailor such a reconnection to be as smooth as possible. This minimizes the risk of “ectopic” pregnancy, which would be very rare in our hands. An ectopic pregnancy occurs when the egg, which is fertilized in the tube, gets stuck at the site of reconnection instead of passing into the womb to begin its growth into a baby. This risk is greatest when the site of reconnection is not a smooth, even transition.
The benefit of using the microscope for this surgery is that we can see the tiny inner opening of the tube clearly, and thereby accurately reconnect it with stitches that are finer than a human hair and literally invisible to the naked eye. A meticulous microsurgical technique is necessary, and this, of course, requires considerable experience. We have performed over 12,000 microsurgical operations to reverse sterility in men and women, after developing these exacting microsurgical techniques on over 2,000 laboratory rats. It requires this kind of extensive practical experience to obtain the best results.
If you have any questions, you may call us at (314) 576-1400.
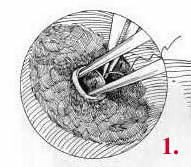
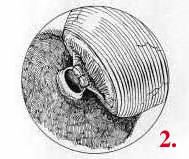

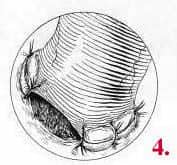
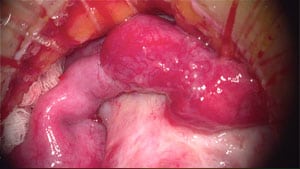
Atlas of photo micrographs of tubal ligation procedures