Unfortunately IVF has become so popular as a treatment for infertile couples, that sometimes without adequate supervision or serious regulation, some small “IVF” centers are opening up in little doctors’ office buildings, and non-experts or newly self-proclaimed “fertility doctors” are delivering the IVF care.
It is best to look for IVF in a setting of a major quality medical center that is more concerned about the practice of good medicine than about your pocketbook and which has invested heavily in high standards “clean room” air purification systems. So you are going to need to do your research.
Learn more about Low Cost IVF
IVF (in vitro fertilization) is the most common form of ART (Assisted Reproductive Technology). If the fallopian tubes are damaged or the sperm is poor, it is obviously the only acceptable treatment. It is also usually the most effective treatment for most other types of infertility as well. The eggs are fertilized in our laboratory, and the resulting embryos then are placed into the uterus 2 to 5 days later. This procedure achieves remarkable pregnancies even in women with hopelessly damaged fallopian tubes, seemingly sterile husbands, and even “unexplained” infertility. Problems with the husband’s sperm are never a serious issue, since we can fertilize the eggs with ICSI. In fact, in our program we routinely use ICSI in all cases to guarantee against any risk of failed fertilization. Our IVF pregnancy rate is over 50% per attempt, regardless of diagnosis, and we accept all of the most difficult cases.
Extra embryos are frozen and saved for a later, much less expensive future pregnancy. Our very special Japanese freezing technique essentially assures no damage to viable embryos. Therefore, the success rate for frozen embryo transfers in our program is just as high as for “fresh” IVF. The cost for subsequent frozen IVF cycles is one quarter the cost of the original cycle, thus easing the economic burden to some degree. See: ART Pregnancy Rates
With IVF, the eggs are fertilized in the laboratory, as opposed to GIFT, which simply leaves fertilization up to nature in the fallopian tubes.
Learn more about IVF for older women
How Does In Vitro Fertilization (IVF) Work?
Eggs are retrieved by ultrasound guided needle aspiration under light sedation (in the operating room). This involves no surgical incision, and virtually no pain afterward. You just leave the hospital directly from the operating room, with no pain, and come back three days later to have the embryo (or embryos) placed very simply into the uterus through the cervix with a tiny catheter. No incision and no anesthetic are needed. An hour later you are able to go home. There is no pain from the procedure.
In order to retrieve these multiple eggs for IVF, the woman must undergo injections with hormones and careful monitoring of her ovaries by ultrasound and her hormone levels by blood tests every day or every other day until she is ready for the egg retrieval. This can at first seem very intimidating, but we will “hold your hand” throughout the whole time and guide you gently through this. There are several methods of hormonal stimulation for IVF, that basically can be divided into what we call “conventional stimulation” and “minimal stimulation,” or “mini-IVF.” We will explain which approach is most suited for your particular situation. Meanwhile you can find out more about this by reading our pamphlet, by watching our ART teaching DVD, or in more depth by ready my book, How to Get Pregnant [links to Amazon.com].
IVF Cost
Since infertility treatment is expensive, we try to soften its impact by achieving the highest possible pregnancy rates, and thus reduce the number of treatment attempts and the overall expense. We also make sure not to charge extra for unnecessary testing or ineffective preliminary treatment approaches. We only recommend what we feel is necessary to help you achieve a pregnancy as soon as possible. Furthermore, we have no hidden extra charges added on which in some clinics might result in much higher costs.
For example, there is no additional charge for office visits, semen analysis and/or sperm freezing, embryo freezing, assisted hatching, blastocyst culture, or ICSI, which we always do in every case to give you the greatest chance for pregnancy. Also, we will not order an expensive list of purely remunerative tests with procedures that just delay the most cost effective treatment.
Couples often ask if there is a discount for subsequent cycles if they don’t get pregnant with the first cycle. With our remarkable vitrification technique or embryo freezing, the pregnancy rate for subsequent frozen embryo transfers is just as high as for fresh IVF, but the cost is only one quarter the cost of a regular IVF cycle. So if we can get high pregnancy rates with the normal IVF cycle, and then even higher pregnancy rates with cheap subsequent frozen embryo cycles, your overall cost is dramatically lowered. Furthermore, our “mini-IVF” technology dramatically reduces your cost as well.
Related Media
See Also
Mini-IVF: Minimal Stimulation IVF Technique
In addition to IVF with conventional stimulation, we also offer IVF with minimal stimulation (mini-IVF), which is a new, dramatically lower cost option with comparable results. Our mini-IVF protocol, first conceived in Japan, is truly an amazing breakthrough.
When patients contemplate IVF, their first reaction is often the fear of daily injections of hormones for months, the incredibly high cost of the drugs, the risk of multiple pregnancy and consequent prematurity, side effects related to high levels of estrogen resulting from large numbers of eggs, hyperstimulation syndrome, and the prospect of painful daily progesterone injections for a full ten weeks even after the IVF procedure. Mini-IVF is a very unique approach developed by our colleagues in Japan (and then perfected in our clinic) to circumvent these problems and to simplify IVF for patients, reducing the cost while maintaining the same success rates. For older patients, the success rate is even higher than with conventional IVF. With the refinements we have added to mini-IVF, the pregnancy rates are startlingly high.
Mini-IVF is designed to recruit only a few (but high quality) eggs, thus avoiding the risks of hyperstimulation, reducing the number of injections and dramatically reducing the cost of medications. In many patients who had very poor quality embryos with conventional IVF stimulation protocols, mini-IVF dramatically improved their embryo quality and resulted in pregnancy in otherwise “useless cases.” This approach is not just a simple-minded reduction in hormonal stimulation. It is an ingeniously conceived and completely different approach to IVF that saves the patient much of the complexity and cost associated with more conventional IVF protocols. Here is how it works:
On Day 3 of the menstrual cycle, you start on a low dose of Clomid (50mg), but you don’t stop the Clomid in five days as is usually the custom. You just keep taking the Clomid until ultrasound monitoring shows the follicles to be ready for ovulation. A very low “booster” dose of gonadotropin (just 150 iµ of FSH), is added on Days 8, 10, and 12. Clomid not only stimulates your own pituitary to release FSH naturally (by blocking estrogen’s suppressing effect), but also staying on the Clomid (a unique new approach) blocks estrogen’s stimulation of LH release, and so also prevents premature ovulation. Thus, with this simple change in protocol, the old-fashioned, cheap Clomid is able to stimulate the development of smaller number of better quality eggs for IVF.
Another advantage of this protocol is that you did not have to go on Lupron first to suppress the pituitary. Staying on Clomid blocks estrogen from stimulating your pituitary to release LH, and this prevents premature ovulation without your having to be suppressed. This means that you can be induced to ovulate with just a simple injection or nasal sniff of Lupron. This causes a more natural LH surge, and avoids the luteal phase defect caused by HCG that would otherwise require months of progesterone injections.
The next step is to recognize that Clomid has a negative effect on the uterine lining (because it prevents estrogen from stimulating the endometrium). That is one reason why results in the past have been so poor with the use of Clomid for ovarian stimulation. The embryos are less likely to implant in such endometrium. But that problem is solved by using the Japanese protocol for embryo freezing, “vitrification.” Using this approach, we can now very safely freeze embryos with virtually no risk of loss. Frozen embryo transfers can then be performed in later natural cycles.
Even for poor prognosis cases of older women with low ovarian reserve, there is an advantage to mini-IVF over high dose stimulation. Such patients normally yield very few eggs even with huge megadoses of gonadotropin. Mini-IVF is just as likely to yield as many eggs (very few, of course) as giving huge megadoses of gonadotropin. But the egg quality is better and they can afford to do more cycles if that is what is required. Even in the worst case scenario, when there are no eggs left at all, then at least the patients can discover this with only about $800 spent on drugs instead of $7,000 (cost of maximum dosage).
Think of this simple parable: If you are sitting under an apple tree, and wish to eat the most ripe and ready apples, you have a choice. You can chop down the tree, and look at every apple on the fallen tree to see which ones were ready. Or you can simply try to shake the lower branches and eat the one or two that have fallen. That is the idea of mini-IVF. For many patients, it will remove much of the aggravation and complexity associated with IVF, and also dramatically reduce the cost. But it requires a great deal of sophisticated ability to do well.
It’s absolutely remarkable how many poor quality eggs are obtained in most conventional IVF cycles and how few of them will ever become a baby. With mini-IVF, we get smaller numbers of eggs, but most of them make perfect embryos. So the pregnancy rate per egg has been shown to be five fold higher with mini-IVF than with conventional stimulation, and the pregnancy rates are just remarkable. Nonetheless for some patients conventional stimulation is preferable in order to get more embryos, and we can explain that to you for your particular case.
Mini-IVF is tricky to perform well and many centers which try it are deficient. There is no margin for error. There are several reasons for the success we have with these much lower cost mini-IVF techniques which we have pioneered in the U.S.Firstly, it is hard to overstate how crucial the purity of air quality in the lab as well as the operating room is. There are organic volatile toxins in the air everywhere in microscopic quantities that don’t seem to affect our well being. But they do dramatically affect the well being of these highly exposed embryos. Secondly, the very clever Japanese approach to minimal stimulation allows us to retrieve smaller numbers of better quality eggs than the more expensive massive dosing of conventional IVF protocols, better quality eggs at lower cost. Finally, the ability to freeze the embryos with impunity and then transfer in a later cycle where the uterine lining is more perfectly synchronized to the stage of embryo development than during a stimulated cycle, all add up to high success rates at lower cost.
Infertile couples from all over the world come to St. Louis, Missouri, to chase their dream, because Dr. Sherman Silber and his team are simply the best there is.
Discovery Health Channel Documentary

Improvements in Embryo Culture
A major improvement in embryo culture was realizing that the oxygen content in the air we breathe is much too high for eggs and embryos. In fact, most cells in the body are exposed to a much lower concentration than the air we breathe. Too much oxygen delivered to these cells can, in a sense, overheat the cell. So it is much better to culture the embryos, not only in 5% CO2, but also in only 5% oxygen (not the 20% that is in air). This is difficult to do. Large amounts of pure nitrogen gas have to be blown constantly through the incubator at a carefully controlled rate to lower the oxygen concentration in the incubator. But it is worth that extra effort to get higher pregnancy rates.
Classically, most IVF labs have cultured embryos at a pH of 7.4 (the normal acid-base of blood concentration), and at an oxygen concentration of 20% (the same as in the air we breathe). However, these are not the acid or oxygen concentrations that are most favorable for embryo growth and development. In fact, the acid concentration inside the embryo is normally much greater than that, and the oxygen concentration is much lower. Conventional IVF culturing conditions, therefore, are too alkaline and too oxygen-rich. In fact, oxygen concentration in the Fallopian tube is only about 8% (not 20% as in air), and in the uterus, it is as low as 2%.
This type of optimal culturing of embryos requires a lot of extra attention. To reduce the oxygen concentration in the incubator from 20% to 5% requires blowing through a huge amount of nitrogen (95%), and to keep the pH acid at 7.2 (but not too acid below 7.2), requires careful monitoring of the acidity of the media. This represents a lot of extra work, but it is well worth the effort. The better your pregnancy rate per cycle, the less is your eventual cost.
In a high quality referral hospital setting such as ours, the most rigid air quality system is in place, preventing particles of volatile organic compounds from entering the environment where your embryos are growing in culture. The air around all of us is filled with these toxic compounds in low concentrations that don’t seem to affect your body’s overall health in any obvious way, but do seriously affect the growth and development of your eggs and your embryos in culture. We can see the obvious negative effect of non-perfect air quality in an IVF lab on the evolution of poor quality embryos that give lower pregnancy rates than the good quality egg and embryo growth from those same women whose embryos are cultured in high air quality environments.
Only large IVF centers in high quality hospitals that invest many millions of dollars into “clean room” air quality, can insure the proper environment for the growth in vitro of your eggs and embryos. Even older women in their late 30’s and 40’s, whose embryos cannot tolerate the slightest stress, develop good quality embryos in a laboratory environment like ours that is free of these common toxins in the air that pervade most office based settings.
Freezing Embryos by Vitrification
This new technique of freezing called “vitrification” avoids the damage caused by ice forming inside the cell by not trying to pull every last molecule of water out, because it is impossible to do this 100%. In fact, 70% of the cell is water, and at best you can reduce that to 30%. So with the conventional controlled rate slow-freezing technique, there is always going to be some intra-cellular ice crystal formation, causing some damage to embryos, and severely damaging most eggs. Vitrification uses a super high concentration of antifreeze (DMSO and ethylene glycol), and drops the temperature so rapidly that the water inside the cell never becomes ice. It just instantaneously super-cools into a solid with no ice crystal formation at all.
We can now freeze and thaw, and even refreeze and rethaw, with impunity, using this new protocol from Dr. Masashige Kuwayama from the Kato Clinic in Tokyo. With conventional “slow freezing,” the temperature of the embryo goes down at precisely 0.3°C per minute. With vitrification (using four times the concentration of antifreeze, or cryoprotectant), the temperature is dropped at 23,000 degrees C° per minute, that is 70,000 times faster. At that speed of cooling, and at that concentration of antifreeze, ice crystals simply cannot form.
Of course, it is not quite as simple as it might sound. Such high concentrations of antifreeze, in a few minutes, could be toxic to cells. Therefore, the embryos (or eggs) must first be placed in lower concentrations of antifreeze (and sucrose to draw some water out), and then left in high concentrations only for less than a minute before instantaneous freezing. Then when the time comes to thaw the embryo, it must be instantaneously warmed, immediately taken out of the high concentration of antifreeze, and then placed into a solution with lower concentration, in order to avoid antifreeze toxicity. This requires more skill than conventional freezing, but it is faster, cheaper, and most importantly, avoids almost all freezing damage to either eggs or embryos. Such a reliable method of embryo freezing gives the IVF program much greater ability to avoid dangerous multiple pregnancy, allows ingenious new protocols like mini-IVF to work with less expense to the patient, allows the patient to have many more chances for pregnancy in subsequent cheaper frozen embryo cycles, and makes scheduling for procedures like egg donation or gestational surrogacy much simpler for the patient.
Using this vitrification technique for freezing, we can now also preserve eggs as well as embryos and sperm. This allows us to preserve the fertility of young women or cancer patients for the future in egg banks if they need to delay childbearing.
Summary of IVF Cost Reduction
There are several ways in which to lower the costs for IVF and improve quality in which we are leaders. There are some clinics that simply charge less by doing slipshod work, and we abhor that. There are many relatively poor quality OB-GYN doctors who have been kicked off of hospital staffs who are opening cheap IVF clinics with the idea or making an easy dollar by cutting quality, and who have little depth of knowledge. We recently performed a successful low cost IVF on a patient who had gone through eleven previous IVF cycle failures at such a bargain rate clinic. She wound up spending a fortune on all these failures before we finally achieved her goal in just one properly performed cycle. We have also seen many patients come from such office IVF settings to our hospital with life threatening hyperstimulation syndrome from poorly managed IVF stimulation and of course they endured a huge hospital bill for the intensive care required to save her life. To avoid such charlatans, you will need to understand and research IVF carefully.
The first requirement is to have the most perfect industrial-grade laboratory conditions. This results in better quality embryos with high pregnancy rates even in patients with otherwise lower prognosis. The second is that with our remarkable freezing technology, considered the best in the U.S., subsequent frozen embryo transfers, which cost very little, will give you even higher pregnancy rates because your endometrial uterine lining is more perfectly synchronized to the stage of embryo development than in a fresh stimulated cycle. Thus you have more chances per retrieval of eggs for pregnancy. The third is that we have developed a novel method of ovarian stimulation that is very mild and less drug intensive called mini-IVF.
Mini-IVF is not suitable for all cases, but it is clearly the least expensive and most comfortable way to undergo IVF. Its only disadvantage is less frozen embryos for future babies, but for many couples that is preferable anyway. But even when conventional stimulation IVF is required or preferred (because of the greater number of embryos), overall cost is reduced because of the technical perfection of our freezing protocol, which results in many more embryos transfer opportunities at dramatically lower cost than a fresh IVF cycle.
The American College of Pathologists (CAP) inspects American IVF labs every two years and issues reports on the IVF laboratory’s quality. Our lab has been rated as one of the very best in the U.S. It is our compulsive attention to quality and detail that produces our great results in some of the most difficult cases, and is why our CAP inspection reports are at the highest possible level. Ultimately these better results are the best method for cost saving.
More details of costs for these different approaches can be discussed with our office personnel after your initial consultation, which is completely complimentary.
Blastocyst Culture — Dr. Silber’s comments
Whenever IVF or ICSI is performed, embryos may be cultured for either one day, two days, or even five days, before transferring them back into the woman. In order to culture the embryos for five days, i.e. to what we call the “blastocyst” stage, you need to use “sequential” culture media systems. We have used such a system since the summer of 1997 because it gives us the option of culturing the embryos for as long as is clinically appropriate for each particular patient’s situation.
However, there is a great deal of debate, and some considerable commercial hype, centering around whether to culture for two days, three days, or five or six days. The media we use, and which many other of the best programs use, allows us to culture the embryos to whatever number of days is appropriate for the particular patient. Since this media is commonly available, it should not be used to hype any particular program.
For some patients with poor quality embryo development (a condition which is programmed into the genome of many infertile women), even with the best culture media, the embryos may be better off going directly into the fallopian tube immediately. For the average patient, day two or day three transfer either to the fallopian tube or to the uterus may be best. For some patients, day 5 transfer to the uterus may be a good option. The problem with extended culture to day 5 is that there may be a loss of some embryos that might have “made it” if they had been transferred earlier.
The major advantage (despite the already mentioned disadvantage) of day 5 transfer is embryo selection. The implantation rate per day 5 blastocyst transfer is greater than for transfer of day 2 or 3 embryos. But only 20 percent to 50 percent of day 2 embryos can develop in vitro to day five no matter how perfect the in vitro culture system. There is a potential loss therefore of what could have been viable embryos. So selection is the only advantage of blastocyst culture, and this selection has nothing to do with the “quality” of the baby, but rather just whether the embryo “makes it” or not to becoming a baby.
Either way, because our system of embryo freezing is so good, we do not lose anything if we transfer less embryos to reduce your risk of triplets or quadruplets, and just save the extra embryos for a later pregnancy. We can even transfer just one embryo at a time (if that is your wish) without at all reducing your chance of pregnancy.
Therefore, hype should be removed from this issue, and decisions should be made that are in the best interest of the particular patient’s situation.
Nonetheless we believe that use of sequential culture media, as we routinely do, is an advantage, in that patients can have the option of prolonged embryo culture if that is in their best interest.
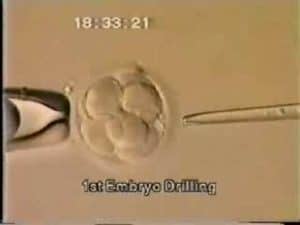
Assisted Hatching
Assisted Hatching: Excerpt from “How to Get Pregnant With the New Technology, Updated and Revised”
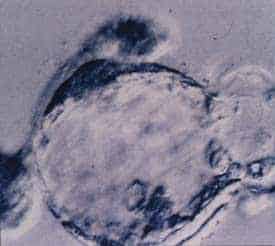
Another attempt at improving the pregnancy rate is the idea of “assisted hatching”. The concept of this procedure is that based on the fact that the embryo normally sits around in the uterus without any effort to implant until around day six. Until day six, the embryo keeps growing within its very tough zona pellucida (outer shell). But on day six, that zona pellucida begins to thin out, and the embryo then eventually “hatches,” just like a chicken out of an egg. It is at this moment of hatching that the embryo, now called a “blastocyst,” actually implants into the uterine lining, the endometrium. It is at this moment, around day seven after fertilization, that pregnancy actually occurs, and this free floating ball of cells finally becomes a part of the mother. One theory to explain the perplexing phenomenon that many IVF embryos do not result in a pregnancy has been that this thinning of the zona and hatching of the embryo may be defective and in some way impeded in embryos that have been cultured in vitro.
The solution to this problem would be to microsurgically thin out the wall of the zona pellucida of these embryos on day three, just prior to transfer. It was hoped that this micromanipulative process to the embryos might provide a necessary extra bit of help to improve the implantation rate. This proposition is very difficult to prove with certainty, but in many centers, including ours, assisted hatching is performed on most embryos, and the results have thereby improved. It is a beautiful procedure and a wonderful rationale, and in women who have failed to get pregnant through the transfer of perfectly good embryos, the standard approach at the present should be to give them the benefit of the doubt, and to do assisted hatching.