Treating Infertility – Dr. Silber
Click Here to download Treating Infertility in PDF format.

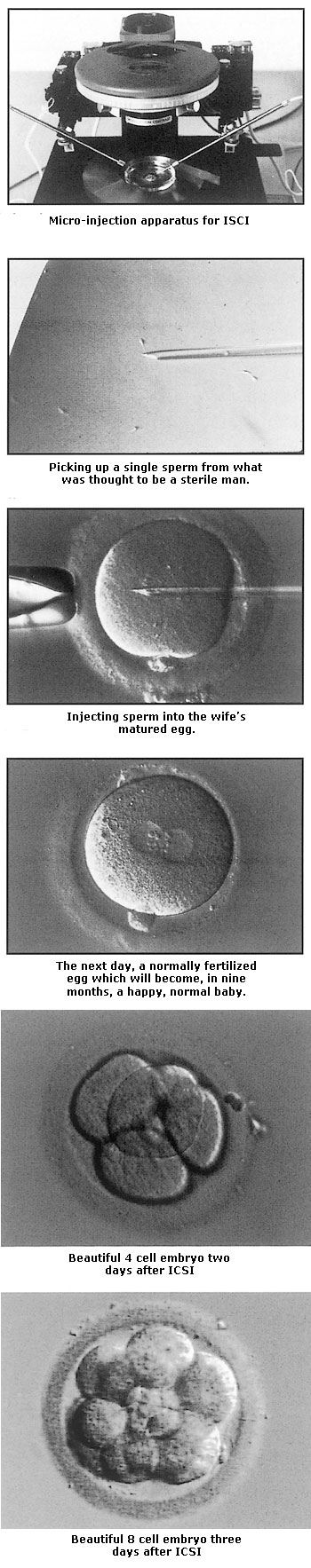
In the early 1990s, the major stumbling block to treatment of infertile couples was the severely infertile male. In about 50 percent of infertile couples, there is a somewhat low sperm count, and in 10 percent the count is extremely low. In such cases, even IVF had routinely failed in the past. There was simply no effective treatment available for the infertile male. That all changed dramatically after 1993, thanks to the pioneering work on sperm retrieval and ICSI performed by Dr. Andre Van Steirteghem, Dr. Paul Devroey, and myself, shuttling back and forth between Brussels, Belgium, and St. Luke’s Hospital in St. Louis. The work of this team has revolutionized the treatment of male infertility throughout the world and represents the single greatest advance in fertility treatment since the first IVF baby in 1978. Now it is possible to search for just a few sperm in the male ejaculate, and if there is no sperm in the ejaculate, often a few can be found in the testicle. We can then inject a single sperm [technical video] into each of the female’s eggs (ICSI). With this delicate technique, we achieve pregnancy rates for virtually sterile men that are no different from that of men with normal sperm counts. There are now very few cases of severe male infertility that cannot be successfully treated.
This is how the technique works: With ultramicromanipulative instruments attached to special microscopes, the woman’s otherwise invisible egg can actually be held secure with a microscope “holding” pipette, and an even tinier micropipette can be used to inject a sperm through the hard outer shell of the egg so that this one sperm is literally forced to fertilize the egg. Can you imagine the delicacy of this type of manipulation? The sperm head is no more than 4 to 6 microns in diameter (that’s approximately 1⁄4,000 of an inch), and an egg is approximately 130 microns in diameter (1⁄200 of an inch). It took years of painstaking research in Brussels and in St. Louis to perfect it.
One of the biggest fears of those of us who were working on microinjection of sperm was that if the sperm couldn’t get into the egg because of poor numbers, poor motility, abnormal shape, or poor maturation, then perhaps they weren’t meant to get in. Perhaps it was naive to think that if such a poor sperm were injected into the egg, the chromosomes would be normal, and that a healthy baby could be obtained from such a procedure. Those fears proved to be completely wrong.
Even poor sperm have normal DNA sufficient for making a normal baby, and the only thing wrong with poor sperm (with an occasional exception) is simply that they cannot get into the egg. The incredible complexity of sperm physiology appears to serve no purpose other than to mechanically get the package of DNA that the sperm contains into the egg. Once that package of DNA is inserted into the egg, all the processes of fertilization and embryo formation leading to a baby can take care of themselves.
Even Men Who Don’t Make Sperm Can Have Children
In 1985, a young couple, both 22 years of age, from New York, came to see me in St. Louis because he had azoospermia (no sperm in the ejaculate) and needed a testicle biopsy to see whether he had an obstruction that could be corrected with microsurgery. In those days, we always prayed that the biopsy would show normal sperm production, because our success rate with microsurgery to correct obstruction in male infertility was over 95 percent. But we could do nothing at that time for couples if the men weren’t making sperm at all.
His biopsy revealed what we call “maturation arrest.” This means that the early precursors for sperm production were present in the testicle, but there was no continuation of sperm production beyond these early stages. This man was by all definitions 100 percent sterile, and it was my unfortunate job to explain to this otherwise wide-eyed, cheerful young couple (who were looking forward so much to having a family) that they couldn’t have children.
But this couple never gave up hope. Ten years later, they came back after they had heard about ICSI. By now we were having exciting success in using ICSI for men with extremely poor sperm counts, and in men with irreparable obstruction requiring retrieval of testicular sperm from a blocked but otherwise normally functioning testicle. But could it possibly work for men who were apparently not making any sperm at all? This determined couple helped us embark upon a new theory with startling consequences.
When I had looked back to my research from the early 1980s on quantitative testicle biopsy, I discovered a phenomenon that had previously eluded my attention. Even in men with zero sperm in the ejaculate, and apparently no sperm production, if one looked carefully throughout the testicular specimens, an occasional sperm precursor could be found that had the same number of chromosomes and the same basic appearance as a normal sperm. Based on this finding, this couple was our first case of a man who appeared to be making no sperm but in whom we were able to find just a few sperm “hiding” in his testicles. We injected these hidden sperm into his wife’s eggs, and normal fertilization occurred. They had a happy baby girl who is now a healthy young woman who is having her own children now.
Another patient treated around the same time had, as a child, undescended testicles that were brought down surgically into the scrotum very late in his childhood. As is often the case with such men, he was clearly producing no sperm. When we operated on his testes to see if any sperm could be found (under the same theory, that any man with a testicle may have some sperm somewhere), indeed we were again able to find just a few sperm. We injected his wife’s eggs with those testicular sperm and again obtained normal fertilization and pregnancy. This young man had been known to be sterile ever since he was a teenager. Yet during extensive exploration of his testicles, we found sufficient sperm to perform ICSI, and he could now have a normal family.
The question that might occur to every such couple is, will my baby be normal? The fear might arise that abnormal sperm in men with low sperm counts will cause a higher risk of producing abnormal babies. We have now studied this in over seven thousand such children born through the ICSI procedure as we performed it, and the news is great.
The children are normal, and there is no greater incidence of chromosomal or congenital abnormalities than in the children of normally fertile couples conceiving without any kind of reproductive treatment. There may be occasional exceptions, but they are related to the age of the wife, not the IVF or ICSI treatment. The offspring are more likely to be infertile (like their parents) but are otherwise normal, healthy children.
Poor sperm production represents up to half of the infertility cases in the world, and in the past it prompted couples to undergo billions of dollars’s worth of ineffective, unscientific, and frankly stupid surgical and hormonal treatment. ICSI now solves that problem in most couples, but a genetic cure would still be preferable. Our research, in conjunction with the human genome project, the Howard Hughes Institute at MIT, the University of Amsterdam, and the Kato Clinic in Tokyo, thus far indicates that sperm production in men is controlled genetically by many different genes on the Y chromosome and elsewhere in the genome. We have now completely sequenced the Y chromosome and have located the areas on the Y chromosome where sperm production in these men is regulated, and we have identified many of the genes that control spermatogenesis. This discovery means that in the future we may have a genetic cure for male infertility, i.e., replacing the missing gene (or genes) so that these men will be able to resume normal spermatogenesis, thereby in the future eliminating the need for ICSI.
