
Featured Article
Fertility Road
May/June 2011
It’s a very familiar, sad story: a woman waits until she finds Mr. Right before embarking on trying for a family. More often than not, by the time she finds him she’s pushing 40 and rapidly losing eggs.
The couple goes to see a fertility expert only to be told the chances of successful IVF are extremely slim, not to mention very expensive. Not wanting to reduce their success rate percentage, a clinic will often refuse to treat such patients despite them having the money and being willing to give it a shot. Those that agree don’t hold out much hope – patients shelling out over £6K (about $9800 USD) on something with a 10% success rate or less.
In this situation clinics will often peddle egg donation as the only successful course of action, and the last resort for having a baby. However most couples would prefer to use their own eggs in order to continue the DNA of them and their partner.
So for many women in the their 40s whose chances of conceiving naturally are almost impossible but who aren’t yet ready to resort to egg donation, expensive, painful and more than likely unsuccessful IVF seems to be the only option. Until now.
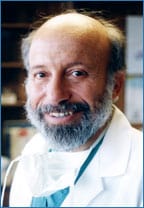
First developed by the Kato Ladies Clinic in Japan, mini-IVF has been perfected and popularised at St. Luke’s Hospital in St. Louis under the guidance of world-renowned fertility pioneer Dr. Sherman Silber. The procedure aims to “tease” the eggs out of older women rather than blasting them out using high doses of hormones. The women embarks on several rounds of this mini-IVF treatment, undertaken back-to-back until four or five good eggs have been retrieved and the same number of embryo’s formed. Only then will the woman undertake the second part of the IVF procedure by having the embryos transferred back.
Not only does this procedure cost less than traditional IVF, the hormone levels required are lower, reducing the need for daily injections and all but eliminating the risk of hyperstimulation syndrome (where the ovaries are overstimulated causing cysts). Hormonal mood swings are also likely to be avoided. “I would like to emphasize that we are not against donor eggs or donor sperm,” says Dr. Sherman Silber in talking about mini-IVF. “We are enthusiasts for this with no waiting list for either, but we recognise that most people would prefer to use their own DNA and, for that goal, properly administered mini-IVF with embryo banking is the best alternative for the older woman or even the younger woman suffering from low ovarian reserve.”
Dr. Silber uses a simple, charming analogy to explain the process to patients in layman’s terms: if you’re sitting under an apple tree and wish to eat the most ripe and ready apples, you have a choice – you can chop the tree down and look at every apple on the floor to see which ones haven’t been damaged, or you can simply shake the lower branches and eat the few that have already fallen naturally. There may be less on the ground but those there will be of a better quality having not hit the ground with force. Replace the apples in this scenario with a woman’s eggs and the tree with a woman’s body and you have the logic behind the concept of mini-IVF.
The Science
This all sounds very easy but in reality mini-IVF is tricky and many centers are unable to perform it successfully as there is absolutely no margin for error. The success of this relatively new treatment, adds Dr. Silber, rests on the purity of air quality in the lab where the embryos are frozen and defrosted, as well as the air quality in the operating theatre. Organic, volatile toxins are present in microscopic quantities in the air – while these do not affect our wellbeing on a day-to-day basis, they do have an adverse effect on embryos, causing damage through over exposure. “We cannot stress how important this is to mini-IVF,” adds Silber.
The very unusual approach to minimal stimulation also plays a very large part in the success of this procedure, with smaller numbers of better quality eggs retrievable through gentler hormone administration – i.e. shaking the tree rather than chopping it down. While less eggs will be retrieved, they have a better prognosis for success.
The storing procedure for the embryos plays the final part in the success of mini-IVF, with vitrification paramount. Vitrification is a new freezing technique that uses super high concentrations of anti-freeze (DMSO and ethylene glycol) to allow a drop in temperature so rapid the water never actually becomes ice. If ice gets into the cells during the freezing procedure, it will damage the cell during the defrosting process. With vitrification, embryos can be frozen and defrosted several times without any risk.
The Procedure
So how do patients interested in mini-IVF go about this procedure and how does it differ from traditional IVF in its administration?
With this more gentle approach, day three of the menstrual cycle is when mini-IVF patients are given low doses of Clomid (50mg). They continue to take this drug until and ultrasound shows there are sufficient follicles ready for ovulation. Staying on Clomid for longer than the usual five days associated with traditional IVF stimulates natural pituitary and releases FSH by blocking the suppressing the effect of estrogen. A very low boost of Gonadotropin is then added on days eight, 10 and 12 of the cycle.
Other than the cost advantages – Clomid is cheaper than those stronger hormones that need to be injected – another advantage is that patients do not need to take Lupron at the beginning of the cycle, rather at the time of ovulation through small injection or nasal sniff. This causes a more natural LH surge and avoids the defects that can be caused by a HCG injection – the ovulation booster used in more traditional IVF.
Patients then embark on several of these treatment cycles back-to-back, waiting until there are sufficient embryos formed before attempting to have them implanted back.
Unfortunately at present time, mini-IVF is only available in the United States, but hopefully Dr. Silber’s work will eventually become more readily available in Europe for older women with fewer egg reserves
Case Studies
We recently took care of such a case in a young woman I had known since she was a little girl,” says Dr. Silber about one of his first mini-IVF patients. “She had undergone multiple surgeries at various clinics for other health problems, but the result of her cure was just one remaining ovary with hardly any eggs left. In fact she did not just want one baby but a big family. The misery this brave young woman had to go through was heartbreaking, being told by everyone that she would never be able to have her own children. We put her through a total of six cycled of mini-IVF, retrieving only a few eggs each time until she eventually had 10 healthy embryos in storage. This resulted in a healthy pregnancy and enough frozen embryos to eventually have the big family she had always dreamed of.
Another example is a 43 year-old woman who married at 38 to a 34 year-old man. She had already conceived naturally before but wanted a second child and was told donor eggs were her only option. Not wishing to have her son’s sibling with a different DNA to his own, she visited St. Luke’s Hospital in St. Louis and went through two rounds of back-to-back mini-IVF cycles, storing up to three embryos, only one of which looked viable. Six months later, the embryo was thawed and transferred back into her uterus for implantation. The patient gave birth to a healthy baby at 44 without the need for donor eggs.
A more determined case was that of a 45 year-old woman who underwent four cycles of mini-IVF stimulation resulting in a healthy 14 embryos. However, as was to be expected due to the age of the embryos, and despite transferring four during the first attempt, the patient failed to get pregnant. However, six months after we thawed and transferred four more embryos, finally delivering a healthy baby using her own eggs at the age of 46. This lady has six frozen embryos remaining meaning it’s possible for her to have a second child in a few year’s time before she reaches the maximum age for treatment of 50. How wonderful would it be for her to able to give birth to a sibling for her first miracle birth?
